Intestinal parasitic infections among children aged 12–59 months in Nyamasheke District, Rwanda
Article information
Abstract
Intestinal parasitic infections are a public health burden and a major cause of illness in developing countries. The diseases lead to various health threats, including growth retardation and mental health-related disorders, especially in children. We assessed the risk factors for intestinal parasitic infections among children aged 12–59 months residing in Nyamasheke District, Rwanda. A cross-sectional descriptive study was conducted using secondary data from 1,048 children aged 12–59 months whose stool samples were examined for the presence of intestinal parasites and whose results were registered in the laboratory information system in 2020. The prevalence of intestinal parasites in children aged 12–59 months was 53.2%. The dominant parasites were Ascaris lumbricoides (13.1%), followed by Giardia lamblia (10.9%), Entamoeba histolytica (7.9%), Trichuris trichiura (6.5%), hookworms (1.7%), and Taenia species (1.4%). A significant association was observed between intestinal parasites and the literacy of mothers or children’s caregivers (odds ratio (OR)=5.09, P<0.001). Children from farming households were 2.8-fold more likely to contract intestinal parasitic infections than those from nonfarming households (OR=2.8, P<0.001). A significant association was also observed between intestinal parasites and food safety (OR=4.9, P<0.001). Intestinal parasitic infections were significantly associated with hand hygiene practices after using the toilet and washing fresh fruits before eating (P<0.001). The information gathered will help public health providers and partners develop control plans in highly endemic areas in Rwanda.
Intestinal parasitic infections are a significant cause of illness and mortality worldwide [1,2]. In developing countries, poor sanitation and sanitary practices increase the risk of contracting these illnesses [3]. Globally, 3.5 billion individuals and 450 million children develop these infections [4]. Children are the most commonly affected age group, and intestinal parasitic infections can affect growth and increase the risk of developing other diseases [5,6]. The common parasites infecting children aged ≤5 years from developing countries include Ascaris lumbricoides, Entamoeba histolytica, and Giardia lamblia [7].
Studies in European countries have reported an intestinal parasitic infection prevalence of 5.9% in children [8]. According to the Association of Southeast Asian Nations, 200 million individuals are infected with soil-transmitted helminths, with A. lumbricoides being the most common [9–11]. In African countries, including Ethiopia and Nigeria, a significant proportion of children contract intestinal parasitic infections, which have long-term effects on physical growth and cognitive and mental development [12,13]. Intestinal protozoan and helminthic infections are prevalent worldwide; however, their distribution varies based on personal and communal hygiene practices, sanitation, and environmental conditions. The World Health Organization (WHO) reported that more than 95% of parasitic infection cases are because of poverty, low income, lack of awareness, illiteracy, improper hand washing following urination, open defecation practices, contaminated drinking water consumption, improper toilet use, improper food handling, and cultural practices [14].
The WHO has set a regular mass drug administration target for all preschoolers and schoolchildren in 46 targeted African countries, including Rwanda, to reduce the burden of intestinal parasitic infections [15]. Despite these efforts to address intestinal parasitic infections, they remain a significant public health concern in Rwanda. In Nyamasheke District, the rate of medication use for intestinal worms was the highest among children aged 12–59 months, as documented in clinical reports from health facilities in 2020. Therefore, intestinal parasitic infections were the major reason for mothers or children to seek medical attention. However, no scientific study has evaluated the prevalence of intestinal parasitic infections and associated risk factors among children aged 12–59 months in the study area.
In this study, we assessed the prevalence of intestinal parasitic infections and associated factors among children aged 12–59 months in Nyamasheke District, Rwanda. This study provides valuable data to help policymakers, decision makers, and program planners successfully implement interventions that can decrease the public health burden.
This study was conducted in Nyamasheke District, Rwanda. Rwanda is located in Central and East Africa. The Nyamasheke District, with a total area of 1,175 square kilometers, is one of the 7 districts in western Rwanda. A large part of this area is surrounded by Lake Kivu, which is the water source of several households. It is composed of 15 administrative sectors, 20 health centers, and 2 hospitals. The Nyamasheke District has an estimated population of 381,804 residents. However, it is predominantly composed of rural areas, and only a small part is composed of small cities (urban areas). The primary sources of income include agriculture, small businesses, and fishing.
This cross-sectional descriptive study used sociodemographic data, hygiene-related behavior, and stool examination results recorded in a laboratory information system in 2020 during the treatment of children. It was conducted among 1,048 children aged 12–59 months. Their stool samples were examined for the presence of intestinal parasites, and the results were recorded in the laboratory information system for 2020. Using the random multistage sampling method, a total of 1,048 children were selected. The laboratory information system comprises data from 20 health centers and 2 hospitals in this district. Forty-five and seventy-four children were selected from each health center and hospital, respectively.
The sociodemographic characteristics, hygiene-related behavior, and stool examination results of 1,048 children aged 12–59 months recorded in a laboratory information system were analyzed. All results recorded in the database (negative or positive) were considered. Intestinal parasitic infections were used as dependent variables, and their associations with sociodemographics, improper food handling, and poor hand hygiene practices were analyzed. To determine participants’ general characteristics, Chi-square test was used. To identify factors associated with intestinal parasitic infections among children aged 12–59 months in this area, binomial logistic regression was used.
Approximately 53.2% of children aged 12–59 months were infected with at least one intestinal parasite (Table 1). The most prevalent helminthic parasite was A. lumbricoides (13.1 %), followed by T. trichiura (6.5%), hookworms (1.7%), and Taenia species (1.4%) (Table 1). The most prevalent protozoan parasites were G. lamblia (10.9%), E. coli (10.5%), and E. histolytica (7.9%) (Table 1).
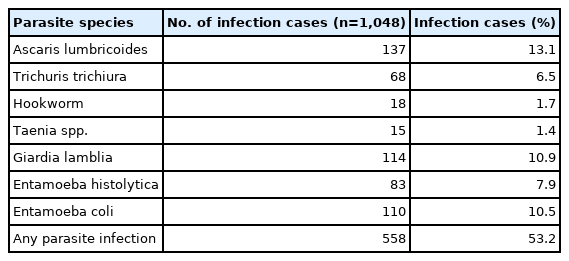
Prevalence of intestinal parasite infections by species in children aged 12–59 months in Nyamasheke District, Rwanda
The sociodemographic characteristics of children aged 12–59 months with intestinal parasitic infections in Nyamasheke District, Rwanda are presented in Table 2. No significant difference was observed in intestinal parasitic infections by place of residence, sex of children, or children’s age group. Of the 1,048 children, 994 lived in rural areas, and 495 (52.4%) were infected with intestinal parasites. Of the 104 children who lived in urban areas, 63 (60.6%) contracted an infection (P=0.114). Approximately 52.9% and 53.6% of male and female children contracted infection (P=0.818). No significant differences were observed in intestinal parasitic infections between children aged 12–23 months (57.6%) and those aged 24–59 months (52.6%, P=0.274).
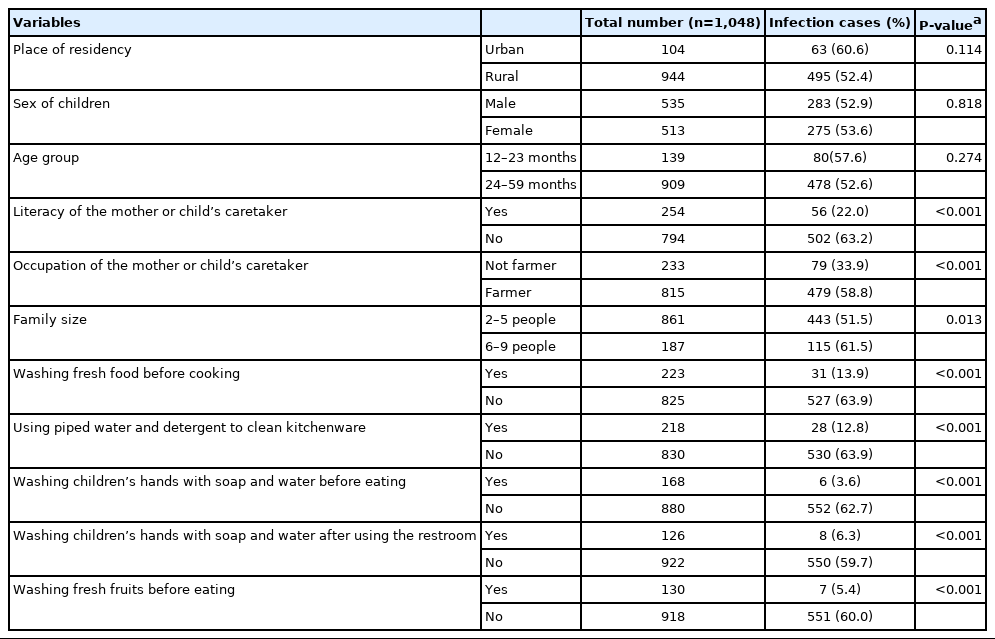
Sociodemographic characteristics of children with intestinal parasite infections in Nyamasheke District, Rwanda
The mothers’ literacy and occupation as well as the family size were associated with parasitic infections in children (Table 2). Approximately 63.2% of children with illiterate mothers (or caretakers) were infected with parasites, whereas only 22.0% of children with literate mothers were infected with parasites (P<0.001). Children whose mothers were farmers (58.8%) had more prevalence of parasitic infections than those whose mothers were nonfarmers (39%; P<0.001). Larger families (6–9 individuals, 61.5%) had a higher proportion of children with parasitic infections than smaller families (2–5 individuals, 51.5%, P=0.013).
Washing hands, food, and using piped water were not performed by most participants, which caused a significant difference in parasitic infection rates among children (Table 2). Only 13.9% of children (31/223) whose mothers responded that they washed fresh food before cooking were infected with parasites, whereas 63.9% of children (527/825) whose mothers responded that they did not wash the food were infected with parasites (P<0.001). Only 12.8% of children (28/218) who used piped water and detergent to clean their kitchenware were infected with parasites, whereas 63.9% of children (530/830) who did not use piped water to clean kitchenware were infected with parasites, as reported by their mothers (P<0.001). Only 3.6% of children (6/168) whose mothers responded that they washed their hands with soap and water before eating were infected with parasites, whereas 62.7% of children (552/880) whose mothers responded that they did not wash their hands with soap and water were infected with parasites (P<0.001). Only 6.3% of children (8/126) who washed their hands with soap after using the restroom were infected with parasites, whereas 59.7% of children (550/922) who did not were infected with parasites, as reported by their mothers (P<0.001). Only 5.4% of the children (7/130) who washed their fruits before eating were infected with parasites, whereas 60.0% of children (551/918) who did not were infected with parasites, as reported by their mothers (P<0.001).
Multivariate logistic regression was performed using variables that showed significant differences (Table 2). The factors associated with the probability of intestinal parasitic infections among children in the Nyamasheke District are shown in Table 3. Children from illiterate families were 5.09-fold more likely to be infected with parasites than those from literate families (odds ratio [OR]=5.09, P<0.001). The mothers’ or child caretakers’ occupation (farmer) was associated with intestinal parasitic infections (OR=2.8, P<0.001).
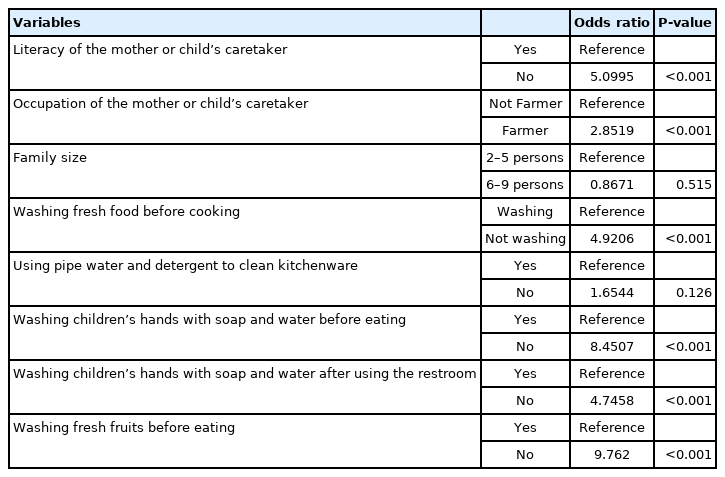
Multivariate logistic regression analysis of intestinal parasite infections with sociodemographic factors
Unwashed fresh food before cooking was associated with intestinal parasitic infections (OR=4.9, P<0.001). Moreover, failure to wash children’s hands with soap and water before eating was associated with intestinal parasitic infections (OR=8.4, P<0.001). Additionally, failure to wash children’s hands with soap after using the toilet was associated with parasitic infections (OR=4.7, 95% confidence interval: 1.9–11.5). Children from households that did not wash fresh fruits before eating were 9.7-fold more likely to contract parasitic infections than those from households that washed fresh fruits before eating (OR=9.7, P<0.001). In the multivariate logistic regression model, family size (P=0.515) and using piped water and detergent to clean kitchenware (P=0.126) were not significant factors affecting the risk of parasitic infections (Table 3).
Of the 1,048 children, 558 (53.2%) were infected with intestinal parasites. Chirdan et al. [16] evaluated the prevalence of intestinal parasites in children attending Day Care Centers in Jos, Central Nigeria and reported that 57.8% of children aged 0–59 months were infected with intestinal parasites. In our study, the most prevalent intestinal parasite was A. lumbricoides (13.1%); this rate is higher than that reported in a study conducted in a metropolitan city of Bangladesh (1.4% prevalence among pediatric patients) [17] and lower than that reported in a study on ascariasis prevalence conducted among children aged 1–5 years in Makurdi, Benue State, Nigeria (18.75%) [18].
Sociodemographic factors, poor hand hygiene practices, and improper food handling were the primary factors that contributed to the highest intestinal parasitic infection prevalence among children aged 12–59 months in the Nyamasheke District. In our study, the prevalence of intestinal parasitic infections was not significantly different in children from rural and urban areas. However, a study conducted in Kassala Town, Sudan reported that children displaced from rural areas (22.2%) had a higher prevalence of infection than those from urban areas (12.9%) [19]. In the present study, children from households engaged in farming activities had a higher prevalence of intestinal parasitic infections. Similarly, a study conducted in Ethiopia reported that children from families engaged in farming activities had a higher prevalence of intestinal parasitic infections than those from families not engaged in farming activities [20].
To increase the adoption of healthy hygiene practices and lifestyles, health education is necessary. In this study, the education of the mother or child caretaker was associated with intestinal parasitic infections. Intestinal parasitic infections were more prevalent in children from illiterate households.
In conclusion, intestinal parasitic infections remain a public health problem in the Nyamasheke District. Health education campaigns on proper handwashing and food handling should be implemented, particularly in rural areas and among illiterate mothers or child caretakers, to decrease the prevalence of intestinal parasitic infections. To explore other factors associated with intestinal parasitic infections in the Nyamasheke District, further studies are also warranted.
Notes
Author contributions
Conceptualization: Evariste H, Yong TS
Data curation: Oh S
Formal analysis: Kim JY
Supervision: Yoon M, Yong TS
Writing: Evariste H, Kim JY
The authors have no conflicts of interest.
