Preventive interventions and diagnostic testing compliance in the management of tropical infections among patients with sickle cell disease in Tanzania
Article information
Abstract
Sickle cell disease (SCD), a genetic hemoglobin disorder, is a major public health challenge in sub-Saharan Africa, particularly in Tanzania, due to its association with high morbidity and mortality from infections. The disease is the leading cause of complications, emphasizing the urgent need for effective preventive strategies and diagnostic protocols. We evaluated the implementation and effectiveness of infection prevention measures and laboratory diagnostic compliance at Nyamagana District Hospital, emphasizing their effects on patient outcomes and survival rates. This retrospective observational study analyzed the medical records of 157 patients with SCD admitted to Nyamagana District Hospital for infection treatment between January 2022 and 2024. The infection profiles, utilization of preventive interventions (recommended drugs, vaccinations, and chemoprophylaxis), and diagnostic laboratory compliance were assessed. Of the 157 participants, 90.4% had at least one infection during their hospital stay, suggesting the vulnerability of this population to infections. Furthermore, malaria emerged as the most prevalent type of infection (40.1%), which is consistent with its endemic status in Tanzania. Other significant infections included unspecified diarrhea (12.5%) and upper respiratory tract infections (10.8%). Despite the high coverage rates of penicillin V prophylaxis (72%) and pneumococcal vaccination (100%), the utilization of malaria chemoprophylaxis and hydroxyurea was low (only 10.8% and 16.6%, respectively). The diagnostic laboratory test compliance, essential for accurate infection management, was moderate at 63.1%, with significant deficiencies in the blood, urine, and stool cultures and antibiotic susceptibility testing. The administration of hydroxyurea significantly reduced malaria prevalence (P=0.005), fewer vaso-occlusive crises (P<0.001), and severe anemia incidence (P=0.034). Thus, enhancing access to preventive measures and improving diagnostic laboratory compliance are crucial steps for reducing infection-related complications among patients with SCD in Nyamagana.
Introduction
Sickle cell disease (SCD) is a hereditary disorder where red blood cells become crescent- or sickle-shaped, causing various acute and chronic complications [1]. It is inherited through autosomal recessive transmission, representing one of the most prevalent genetic disorders globally, with approximately 300,000 births with SCD annually [2]. The inheritance of two mutated alleles causes SCD, which is characterized by varying amounts of chronic hemolytic anemia, severe pain, and various health-related issues, such as heightened vulnerability to infections, strokes, lung problems, spleen dysfunction, and bone complications [3]. Patients with SCD have a high risk of severe, life-threatening septicemia caused by encapsulated organisms due to splenic dysfunction and are susceptible to several types of infection, including bacterial infections (pneumonia, meningitis, septicemia, and osteoarticular infections), parasitic infections (malaria), and viral infections [4].
SCD is a common inherited disease and a leading cause of noncommunicable deaths globally, particularly in African countries [5]. Malaria remains highly prevalent across sub-Saharan Africa and continues to pose major public health challenges in tropical, resource-limited settings [6,7]. SCD is also prevalent in malaria-endemic tropical regions, wherein insufficient resources contribute to poor health outcomes and high mortality rates among children aged <5 years [8].
Despite limited research on actual sickle cell anemia mortality in Africa, studies have shown that this largely neglected disease has an extremely high mortality rate of between 50% and 90% in children aged <5 years, mainly caused by infectious diseases and severe anemia [9]. In low- and middle-income countries, infection is primarily responsible for most SCD-related deaths due to increased pathogen exposure, comorbidities such as malnutrition, lower vaccination rates, and limited access to essential care, including antibiotics and blood transfusions [10].
Tanzania has the fourth-highest number of births with SCD, followed by Nigeria, Congo, and India [11]. The birth prevalence of SCD in rural Tanzania is exceptionally high, and community awareness is low, with minimal laboratory diagnosis capacity as in most sub-Saharan countries [12]. Although improved care for SCD in Tanzania has increased the lifespan of affected individuals, most are facing health challenges, including susceptibility to infections [13].
Due to compromised spleen function, patients with SCD tend to be susceptible to infections caused by encapsulated bacteria, such as Streptococcus pneumoniae and Haemophilus influenzae [14]. Preventive measures, including early diagnosis, education, and prophylaxis, are crucial in reducing preventable deaths in this population [15]. Furthermore, immunization and antimicrobial prophylaxis could potentially reduce the complications, with significant clinical trials advocating for the cessation of antimicrobial prophylaxis by age 5 [16]. The universal implementation of infection prevention through active, targeted vaccination and routine antibiotic prophylaxis has been considered a challenge in low-income settings [17].
The complexity of SCD requires specialized, multidisciplinary care to treat disease complications and promote optimal clinical results [18]. Hence, the timely and accurate communication of the clinical laboratory test results is important to ensure diagnostic accuracy, as these tests provide essential data for an accurate medical diagnosis [19].
Previous studies have proven the effectiveness of preventive interventions and diagnostic testing in reducing morbidity and mortality among patients with SCD [3,20]. Nevertheless, context-specific data from sub-Saharan Africa, particularly Tanzania, where systemic health infrastructure limitations frequently hinder the implementation of World Health Organization–recommended strategies, has been limited [21,22]. Most existing evidence comes from high-income countries with reliable access to hydroxyurea therapy, prophylactic antibiotics, diagnostic tools, and immunization programs [23].
To address this limitation, the present study provides a real-world evaluation of infection prevention and diagnostic practices among hospitalized patients with SCD at Nyamagana District Hospital, a high-burden, resource-constrained setting. By analyzing the clinical records on prophylactic interventions, immunization coverage, and diagnostic compliance, this study contributes localized evidence to inform national policy and support the alignment of healthcare delivery with international standards. Furthermore, the observed association between hydroxyurea use and improved clinical outcomes reinforces global advocacy for equitable access to essential therapies in similar low-resource environments [24].
Materials and Methods
Ethical statement
This study was conducted in accordance with the ethical principles to protect the participants’ rights and privacy. Ethical approval was obtained from the Institutional Review Board of Tanzania’s National Health Research Ethics Committee (No. NIMR/HQ/R.8a/Vol. IX/4805). The hospital administration granted access to the records with approval from the District Medical officer of Nyamagana District Hospital, ensuring compliance with local data privacy regulations. The data that has been used is confidential due to the sensitive nature of the questions asked in this study, hospital data records were assured raw data would remain confidential and would not be shared.
Study design
This study applied a retrospective observational approach, reviewing medical records from Nyamagana District Hospital. The primary focus was patients with SCD and related infections admitted between January 2022 and 2024. The study objective was to analyze the infection patterns, evaluate the effectiveness of preventive measures, and assess compliance with the infection diagnostic protocols.
Study participants
This study included 157 participants with confirmed SCD diagnoses who were hospitalized due to infections and other medical conditions between January 2022 and 2024. SCD was confirmed based on medical records, primarily a previous history of hemoglobin electrophoresis conducted at Bugando Medical Center. Furthermore, patients with incomplete records or without confirmed SCD were excluded.
Data collection
This study relied on paper-based medical records retrieved manually from the hospital’s registry department, inpatient wards, and the Sickle Cell Special Register, which is a hospital-based register for managing records of patients with SCD. Each patient file typically included demographic details (age, sex, and residence), medical histories including confirmed SCD diagnosis, hospitalization information (admission date, clinical presentation, and discharge summary), laboratory test results, and treatment or medication.
Malaria diagnosis was based on positive rapid diagnostic tests and blood smear microscopy, as documented in the patient records. Urinary tract infections were diagnosed based on the presence of pus cells on urine microscopy. The diagnosis of pneumonia, unspecified diarrhea, and pyrexia of unknown origin was based on clinical evaluation and documentation in the absence of laboratory confirmation in accordance with the established hospital protocols.
Preventive prescriptions such as hydroxyurea, folic acid, and prophylactic antibiotics were recorded in the Sickle Cell Special Register. The nutritional status was assessed using anthropometric measurements such as weight and height, which were routinely recorded in the register. The classification of nutritional status was performed in accordance with the World Health Organization growth standards and malnutrition criteria.
Residential areas were classified as urban or semiurban based on their proximity to major healthcare facilities and infrastructure development. Certain areas, such as Butimba, Iseni, Nyegezi, Mkolani, and Buhongwa, were classified as urban because of their closeness to Nyamagana District Hospital, Bugando Medical Center, and specialized clinics. In contrast, other areas, such as Sahwa, Isebanda, Lwanhima, and Bulale, were considered semiurban because of their greater distance from referral hospitals and limited health infrastructure.
Data analysis
Descriptive statistics were used to summarize the sociodemographic characteristics of the patients, their infection profiles, and the coverage of preventive interventions. The infection frequencies between the different intervention groups were compared using chi-tests, while the factors associated with the occurrence of infection were determined through logistic regression analysis. The model adequacy in the logistic regression analysis was evaluated using the Hosmer-Lemeshow goodness-of-fit test to assess the correspondence between the observed and predicted outcomes. The explanatory power of each model was further assessed using Nagelkerke’s R2, providing an estimate of the proportion of variance in the dependent variable explained by the set of predictors. Furthermore, statistical analyses were performed using Jamovi version 2.3.28, with a significance threshold of P<0.05.
Results
Social demographics and clinical and laboratory characteristics of the study participants
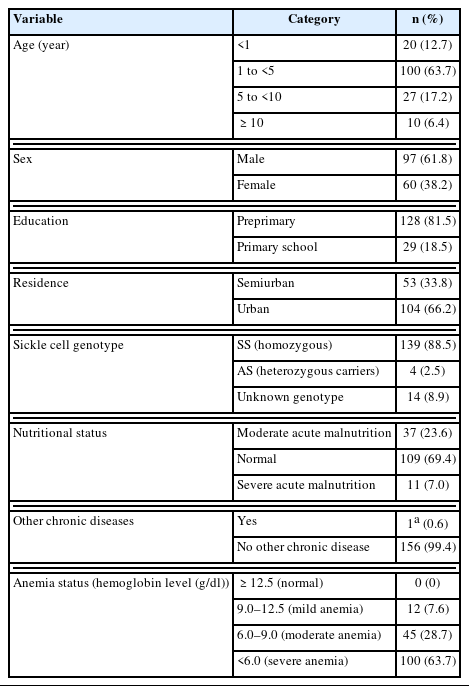
This study analyzed 157 participants, primarily children aged 1–5 years (63.7%), with a smaller proportion of the participants aged <1 year (12.7%) or >10 years (6.4%). Males comprised 61.8% of the group, and most lived in urban areas (66.2%). Most (81.5%) were in early childhood education or had not started formal education. Clinically, 88.5% had the sickle cell genotype SS (homozygous for the sickle cell gene), with a small percentage (2.5%) having the AS genotype (heterozygous carriers). Moreover, 23.6% were classified as moderately malnourished, whereas 69.4% had a normal nutritional status. Only 1 participant (0.6%) had a chronic condition identified as a human immunodeficiency virus infection. Most participants had varying degrees of anemia, with none having normal hemoglobin levels (Table 1).
Infection profile
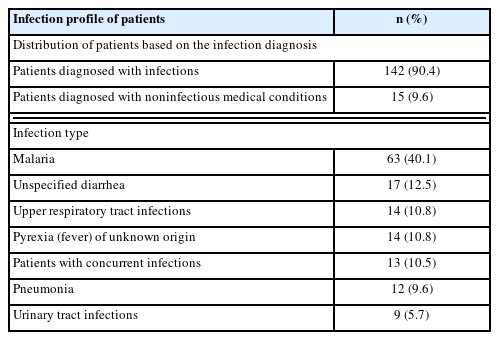
The results indicated a substantial burden of infections among the study population, with 90.4% of the 157 participants diagnosed with at least one infection during their hospitalization. Malaria was the most common infection, affecting 40.1% of the children, followed by unspecified diarrhea (12.5%), upper respiratory tract infections (10.8%), pyrexia of unknown origin (10.8%), pneumonia (9.6%), and urinary tract infections (5.7%). Furthermore, coinfections were observed in 10.5% of the patients, adding complexity to the clinical management (Table 2).
Coverage of infection prevention interventions among patients with SCD
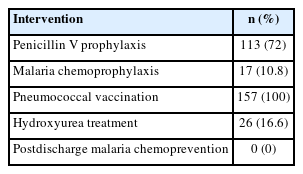
In a cohort of 157 patients with SCD, most of them underwent preventive interventions for various infections. Specifically, 113 patients (72.0%) underwent penicillin V prophylaxis, while 17 patients (10.8%) underwent malaria chemoprophylaxis. All 157 patients (100%) received pneumococcal conjugate vaccine immunization. However, only 26 patients (16.6%) were treated with hydroxyurea. All 157 patients (100%) did not undergo postdischarge malaria chemoprevention after treatment completion (Table 3).
Effectiveness of the infection prevention interventions
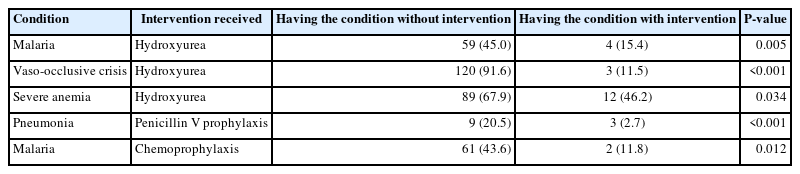
The chi-square test results showed that the patients who were administered hydroxyurea had lower prevalence rates of malaria, vaso-occlusive crisis, or severe anemia than those who did not receive it, indicating statistically significant reductions (P=0.005, P<0.001, and P=0.034, respectively). Similarly, the administration of penicillin V prophylaxis significantly reduced the prevalence of pneumonia (P<0.001), while malaria chemoprophylaxis significantly lowered the incidence of malaria in patients (P=0.012) (Table 4).
Analysis of the factors associated with health conditions among patients with SCD using binomial logistic regression
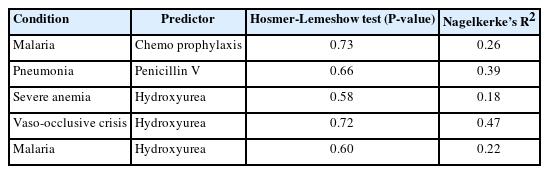
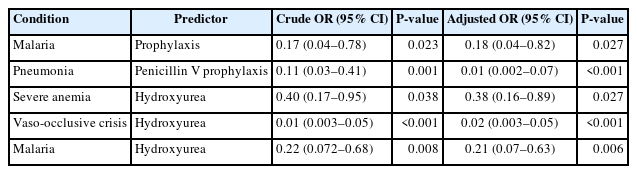
The regression analysis revealed the effects of various predictors on health conditions among patients with SCD admitted to Nyamagana District Hospital. Malaria prophylaxis significantly reduced the odds of developing malaria (adjusted odds ratio (OR)=0.18; 95% confidence interval (CI)=0.0393–0.824; P=0.027). Similarly, penicillin V prophylaxis was strongly associated with a lower risk of pneumonia (adjusted OR=0.0114; 95% CI= 0.00186–0.070; P<0.001). Hydroxyurea has been shown to exhibit protective effects against severe anemia (adjusted OR=0.379; 95% CI=0.1607–0.895; P=0.027), vaso-occlusive crisis (adjusted OR=0.0119; 95% CI=0.00302–0.047; P<0.001), and malaria (adjusted OR= 0.206; 95% CI=0.0668–0.632; P=0.006). These results emphasized the effectiveness of these treatments in reducing the likelihood of these health conditions (Table 5). The goodness-of-fit analysis for logistic regression models predicting health conditions among patients with SCD showed adequate model fit based on the Hosmer-Lemeshow test (P>0.05 for all models) and explanatory power as assessed using Nagelkerke’s R2. Table 6 shows the detailed values.
Binomial logistic regression analysis of the factors associated with health conditions among patients with sickle cell disease
Gaps in diagnostic testing compliance among patients with SCD
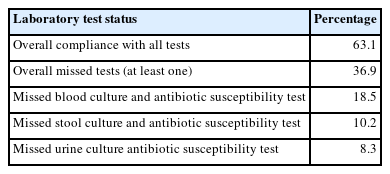
The results revealed significant gaps in diagnostic testing compliance among patients with SCD, with an overall compliance rate of only 63.10%. Over one-third of the patients had insufficient results for at least one critical test, leading to potential delays or missed diagnoses. Particularly high rates of missed tests were observed for blood culture and antibiotic susceptibility test (18.5%), stool culture and antibiotic susceptibility test (10.20%), and urine culture and antibiotic susceptibility test (8.30%) (Table 7).
Discussion
This study highlighted a substantial infection burden among patients with SCD admitted to Nyamagana District Hospital, of whom 90.4% were experiencing infections, primarily malaria (40.1%). The findings of this study are consistent with those of previous studies emphasizing the susceptibility of patients with SCD to infections due to compromised immunity and the high prevalence of malaria in endemic regions [25,26]. Preventive interventions, such as penicillin V prophylaxis and pneumococcal vaccinations, effectively reduced the infection rates. However, gaps were evident in malaria chemoprophylaxis and hydroxyurea usage. Only 10.8% of the patients received malaria chemoprophylaxis, whereas hydroxyurea usage was 16.6% [27], reflecting barriers to comprehensive infection prevention in this population.
In this study, hydroxyurea usage was associated with a reduced risk of malaria infection among patients with SCD. Similarly, previous research reported that hydroxyurea treatment is linked to a lower incidence of malaria in patients with SCD, suggesting its beneficial role in malaria-endemic regions [28]. However, the mechanisms underlying the protective effect of hydroxyurea against malaria may be multifactorial. Hydroxyurea induces fetal hemoglobin production, which increases red blood cell flexibility and reduces sickling. This reduction in red blood cell sickling can potentially lower the sequestration of red blood cells infected with Plasmodium falciparum [29]. Moreover, hydroxyurea has been shown to exhibit mild immunomodulatory properties, which may enhance the body’s immune response to infections, including malaria [28]. Another study also suggested that hydroxyurea may directly affect the malaria parasite’s ability to mature within red blood cells, reducing the parasitemia levels of treated patients [30].
The study also emphasized the significant gaps in diagnostic compliance, with only 63.1% compliance with essential diagnostic testing. Over one-third of the patients lacked results for at least one critical test, posing a risk of undiagnosed or misdiagnosed infections. The high rates of missed tests were observed in the blood, stool, and urine culture and antibiotic susceptibility tests (18.5%, 10.2%, and 8.3%, respectively). Moreover, the frequent occurrence of unclear diagnoses, such as unspecified diarrhea (12.5%) and pyrexia of unknown origin (10.8%), further emphasized the need for strict compliance with the diagnostic protocols. These findings are consistent with challenges in low-resource settings, as observed in Zambia and Congo, where preventive care and diagnostic support remain limited [31,32].
Low compliance with laboratory testing reflects the missed opportunities for timely infection management, potentially leading to adverse outcomes among patients with SCD. Some diagnostic tests were not consistently performed, resulting in critical gaps in laboratory testing compliance. These gaps were then primarily attributed to resource constraints, including the limited availability of reagents, shortage of skilled laboratory personnel, and infrastructural factors, which occasionally resulted in a reliance on clinical judgment in the absence of laboratory confirmation. Thus, strengthening the laboratory infrastructure and ensuring consistent diagnostic protocols could substantially improve infection control outcomes, providing a framework for the better management of patients with SCD in similar healthcare settings.
However, this study has several limitations. A retrospective design was used, which relied on existing medical records that may have been affected by documentation errors or incomplete entries. Missing data related to laboratory results and follow-up prescriptions, may have led to underestimating the infection burden and the coverage of preventive interventions. The study’s single-center setting at Nyamagana District Hospital also compromises the generalizability of the findings to other regions or healthcare contexts. Furthermore, the absence of data on the malaria parasitemia levels and outcomes among patients with no SCD constrained broader comparative analysis. Potential selection bias may have occurred because only patients with confirmed SCD and complete medical records were included. Despite these limitations, our study provides one of the few real-world evaluations of infection management in patients with SCD in Tanzania, providing context-specific insights that can guide future interventions and health policy development in similar settings.
This study has proven that hydroxyurea, malaria prophylaxis, and penicillin V prophylaxis are associated with reduced risks of key health complications in patients with SCD, including malaria, pneumonia, severe anemia, and vaso-occlusive crisis. Improving the health outcomes for individuals with SCD requires expanding access to infection prevention strategies, particularly hydroxyurea therapy and comprehensive malaria chemoprophylaxis in endemic regions. Furthermore, enhancing diagnostic compliance and laboratory infrastructure is essential for timely and accurate infection management, which can reduce missed diagnoses and improve overall patient care.
Notes
Author contributions
Conceptualization: Kim JY
Data curation: Mgasa A
Formal analysis: Mgasa A
Methodology: Oh S
Project administration: Mgasa FP, Kang S
Resources: Mbugi E
Validation: Oh S
Writing – original draft: Mgasa FP, Kim JY
Writing – review & editing: Kim JY
Conflict of interest
The authors declare no conflict of interest related to this study.
Acknowledgments
This study was funded by the National Research Foundation of Korea (NRF) through grants from the Korea government (MSIT) (Grant No. RS-2024-00456300). The authors thank the dedicated staff at Nyamagana District Hospital and the data collection team.