Cerebellar Schistosomiasis: A Case Report with Clinical Analysis
Article information
Abstract
The authors report here a rare case of cerebellar schistosomiasis identified by pathological diagnosis, lacking extracranial involvement. The clinical symptoms included headache, dizziness, and nausea. Studies in blood were normal and no parasite eggs were detected in stool. Computed tomography of brains showed hypodense signal, and magnetic resonance imaging showed isointense signal on T1-weighted images, hyperintense signal on T2-weighted images, and intensely enhancing nodules in the right cerebellum after intravenous administration of gadolinium. A high-grade glioma was suspected, and an operation was performed. The pathologic examination of the biopsy specimen revealed schistosomal granulomas scattered within the parenchyma of the cerebellum. The definitive diagnosis was cerebellar schistosomiasis japonica. A standard use of praziquantel and corticosteroid drugs was applied, and the prognosis was good. When the pattern of imaging examinations is present as mentioned above, a diagnosis of brain schistosomiasis should be considered.
INTRODUCTION
Schistosomiasis is one of the most widespread parasitic infections in the world. Schistosomiasis is transmitted to humans by skin contact with infected water. Three major schistosome species known to infect humans are Schistosoma haematobium (endemic in Africa and the eastern Mediterranean), Schistosoma mansoni (endemic in Africa, the Middle East, the Caribbean, and South America), and Schistosoma japonicum (endemic mainly in China, Japan, and the Philippines). It is estimated that more than 1,000,000 people in China are presently infected with S. japonicum [1,2]. Although gastrointestinal system involvement with S. japonicum appears to be common, brain schistosomiasis is rare. In addition, almost all brain schistosomiasis japonica are accompanied with hepatosplenomegaly.
The authors describe here a case of cerebellar schistosomiasis japonica, predominantly involving the cerebellum, identified by pathological diagnosis, without any evidence of extracranial involvement detected by routine blood, cerebrospinal fluid (CSF), and stool examinations, chest radiograph, and abdominal sonography. This kind of clinical case is possible to occur but has not been reported in the literature with recent retrieval. The patient came from Ganzi region, Sichuan province, one of the severe endemic areas of schistosomiasis in China [3].
CASE RECORD
A 64-year-old, right-handed, herdsman was admitted to a hospital with mild headache, dizziness, and nausea for a few weeks. No fever, convulsion, or any other symptoms were accompanied. The herdsman came from Ganzi region in Sichuan province, an endemic area of S. japonicum in China. His medical history was unremarkable. During the previous few weeks he had experienced intermittent episodes of headache and nausea. On admission he was found to have slow mental functions, but no major neurologic dysfunction was detected. Laboratory findings revealed a leukocyte count of 13,000/ml, a normal RBC count, and no eosinophilia. The CSF revealed normal levels of protein, glucose, and chloride. Other studies in blood and CSF were normal. No parasite eggs were detected in stool. The results of chest radiography and abdominal ultrasonography were normal. Computed tomography (CT) of the brain showed edema areas in the right cerebellum (Fig. 1A). Brain magnetic resonance (MR) imaging was performed later and revealed isointense signals on T1-weighted images (Fig. 1B), hyperintense signals on T2-weighted images (Fig. 1C), and intensely enhancing nodules in the right cerebellum after intravenous administration of gadolinium (Fig. 1D).
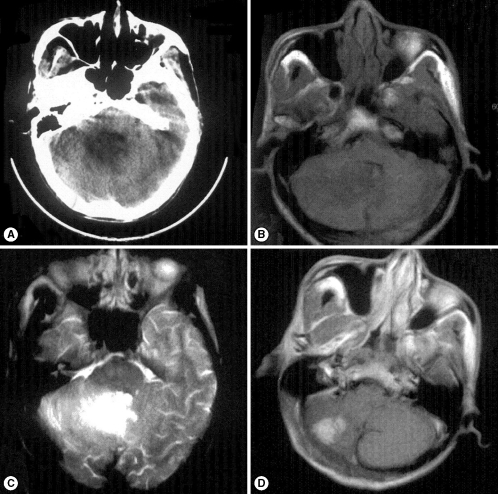
Imaging examinations of the cerebellum. (A) Noncontrast axial CT of the brain showing edema areas in the right cerebellum, (B) Axial T1-weighted MRI of the brain showing isointense signal in the right cerebellum, (C) Axial T2-weighted MRI of the brain showing hyperintense signal in the right cerebellum, (D) Axial T1-weighted MRI after gadolinium injection showing intensely enhancing nodules in the right cerebellum.
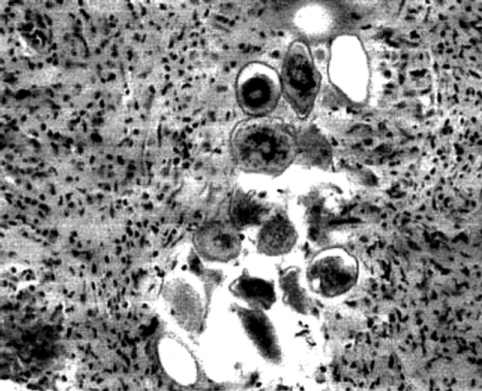
The herdsman was treated with antibiotics for 14 days as the tendentious diagnosis of atypical brain abscess, but still complained of dizziness and aggravating headache. Then a high-grade glioma was suspected, and an operation of total resection was performed to solve the mass effect and intracranial hypertension. However, the examination of a frozen section of the biopsy tissue specimen suggested S. japonicum ova and granulomas (Fig. 2). Pathologic examination of the biopsy specimen revealed sclerosing schistosomal granulomas scattered within the parenchyma of the cerebellum. The diagnosis was confirmed, and the patient was treated with praziquantel at the dose of 20 mg/kg per day for 6 days, with concurrent administration of dexamethasone. The patient was discharged after 24 days and he was followed up 3 months later with complete resolution of the symptoms. However, the patient was lost to follow-up after a period of 6 months.
DISCUSSION
Archeological studies have revealed that S. japonicum has a very long history in China. Schistosome eggs were identified in a female corpse dating back to the Western Han Dynasty some 2,100 years ago that was exhumed in 1971 in Hunan province. Schistosome eggs were also found in the liver of another corpse buried 100 years earlier in Jianglin Hsien, Hubei province. In old volumes of traditional Chinese medicine, a description of clinical symptoms resembling Katayama fever (acute schistosomiasis) can be traced back to 400 B.C. [3].
As mentioned above, 3 major schistosome species are known to infect humans. S. haematobium affects urinary tract predominantly, whereas S. mansoni and S. japonicum characteristically cause intestinal and hepatosplenic diseases. Central nervous system involvement is a rare ectopic manifestation of schistosomiasis. It has been explained that the schistosome eggs are small and could reach the brain easily. The brain disease is caused by the host reaction to schistosome eggs. Some persons with eggs in the central nervous system develop no symptoms. The mechanism of egg deposition is unknown, but their presence suggests that eggs may cross the blood-brain barrier or that some worm pairs may reach the venous side of the brain circulation [4].
The clinical manifestations of brain schistosomiasis are varied. Headache, papilledema, visual abnormalities, and seizure are common manifestations in cerebral schistosomiasis, while nausea, vomitting, brain hernia, and ataxia are more common in cerebrellum and brainstem schistosomiasis. As the cerebellum is rather smaller than the cerebrum, emergency operations of total resection or partial resection should be introduced to control critical intracranial hypertension and potential hernia in the cerebellum, while drug intervention and dehydration treatment are usually adequate for cerebral lesions. Duration of the symptoms varies from a few weeks to more than 1 year [5]. The presentation in pediatric patients is very similar to that observed in adults [6]. Some studies suggested that seizure is common in the chronic stage, whereas there is increased intracranial pressure in the acute stage [7].
The diagnosis for brain schistosomiasis is difficult, as clinical findings are non-specific and laboratory changes such as eosinophilia and evidence of schistosome ova in stool or urine may or may not be present. Neuroimaging examinations can give significant help. The leptomeninges and cerebral cortex are the most common sites involved, whereas the cerebellum, thalamus, hippocampus, midbrain, basal ganglia, choroid plexus, and white matter are less frequently involved. In the mass form of brain schistosomiasis, CT typically reveals a nodular, enhancing, space-occupying lesion with surrounding edema, and contrast-enhanced T1-weighted MR images in many patients revealed a central linear enhancement surrounded by multiple enhancing punctate nodules, forming an "arborized" appearance. Pathologically, this enhancement pattern correlated with a host granulomatous response to schistosome eggs. Although the pattern is not present in all cases of brain schistosomiasis, when it is observed, a diagnosis of brain schistosomiasis should be considered [8].
Epidemiologic history in combination with positive results of cerebrospinal fluid ELISA and the patient's recovery after chemotherapy can establish the diagnosis, although biopsy of the intracerebral lesions may be considered [9,10]. However, the history of exposure to schistosome infected water is important for the diagnosis. The prognosis of schistosomiasis depends on early diagnosis and good treatment.