Use and Effects of Malaria Control Measures in Pregnancy in Lagos, Nigeria
Article information
Abstract
In Nigeria, malaria causes up to 11% of maternal mortality. Our main aim was to find out the most common mosquito control measures employed by the pregnant women in Lagos and their effects on malaria infection. The study was carried out over a period of 6 months during which trained interviewers administered questionnaires to 400 pregnant women. The prevalence of malaria was 8.4%. There was no significant association between the prevalence of malaria and age, level of education, or occupation of the participants. Pregnant women in the age range 26-30 had the mean parasite density (409.9±196.80). Insecticide spray (32.8%), mosquito coil (27.5%), and insecticide-treated nets (ITN) (15.5%) were the major mosquito control measures employed by the participants while the prevalence of infection among them were 2.3%, 6.2%, and 3.2%, respectively (P<0.05). Only 18.3% of the women had taken more than one dose of intermittent preventive treatment (IPT), while another 11.8% had taken a single dose. The infection rate among them was 4.1% and 6.4%, respectively. Malaria prevalence was highest among those who had not received any dose of IPT (10%). This study showed that the use of ITN and IPT among the pregnant women were still unacceptably low. It also showed that the use of insecticide spray which was the most common malaria control measure adopted by the participants was effective despite the fact that it is not a National Malaria Control Policy. We recommend that a sustained integrated mosquito management and public education should be strengthened in Nigeria.
INTRODUCTION
Malaria is caused by the parasite of the genus Plasmodium which is usually transmitted by the bite of an infected female anopheles mosquito. Plasmodium falciparum is the commonest species in Africa, and it accounts for up to 98% of the cases in Nigeria. Other species include P. malariae, P. ovale, and P. vivax. Malaria is endemic in most parts of Nigeria with stable transmission all year round. High temperature, humidity, and rainfall are some of the factors that enhance mosquito breeding and malaria transmission [1]. Some of the major Anopheles species that transmit malaria in Nigeria are An. arabiensis, An. brochieri, An. coustani, An. flavicosta, An. funestus, and An. gambiae.
This disease remains one of the most terrible public health problems in Nigeria, causing about 60% of all outpatient attendances and 30% of all hospital admissions. It is responsible for nearly 110 million clinical cases and an estimated 300,000 deaths per year, including up to 11% of maternal mortality. Also, malaria's economic impact is enormous with about N132 billion lost to malaria annually in form of treatment costs, prevention, loss of man hours, and so on [2]. Pregnant women and children below the age of 5 years bear the greatest burden of malaria in Nigeria, like many other endemic regions in Africa. Malaria in pregnancy was believed to contribute to 3-5% of maternal anemia, 8-14% of low birth weight (LBW), and 3-8% of infant mortality [3]. In south-west Nigeria, past studies reported malaria parasite prevalence between 60% and 72% among pregnant women [4,5].
Malaria programme coverage has increased substantially across Nigeria from 1991 to date. However, current coverage levels remain considerably under the targeted 60% levels established in the previous plan and far below the levels (>60% coverage) at which major impact of the interventions on malaria burden would be expected [2]. In a study carried out to evaluate the ownership and use of insecticide-treated nets (ITN) in Nigeria, Senegal, Uganda, and Zambia between 2000 and 2004-2006, it was observed that there were large increases in the ownership in all countries. All countries but Nigeria made commensurate gains in the proportion of under-fives sleeping under a net/ITN, and in all countries the proportion of pregnant women sleeping under a net/ITN increased greatly, but none of the countries reached the ambitious Abuja targets for ITN use [6].
The efficacies of using indoor residual spray (IRS) and ITN against malaria vectors were compared (using data from 6 recent comparisons in Africa, Asia, and Melanesia). By all the entomological and malariological criteria recorded, pyrethroid-treated nets were at least as efficacious as house spraying with dichlorodiphenyltrichloroethane (DDT), malathion, or a pyrethroid. However, when data from carefully monitored house spraying projects carried out between the 1950s and 1970s at 3 different locations, including Garki (Nigeria) were compared with insecticide-treated net trials with apparently similar vector populations, the results with the ITN were much less impressive. The possible explanations for this observation was said to include the longer duration of most of the earlier spraying projects and the use of non-irritant insecticides. Non-irritant insecticides are likely to kill mosquitoes more than the irritant pyrethroids, which tend to make insects leave the site of treatment (i.e. are excito-repellent) [7].
World Health Organization (WHO) currently advocates the use of Integrated Malaria Management (IMM) as the most effective tool to check the menace of malaria [8]. IMM consists of 3 tools: effective case management (ECM), integrated vector control (IVC), and personal protection (PP). These tools have to be applied simultaneously to be able to produce the desired impact. ECM is the use of effective antimalarial drugs to remove parasites from infected human hosts thereby preventing transmission to mosquitoes [9,10]. IVC is the use of adult mosquito killing measures, such as indoor insecticide sprays [11], and environmental management to remove the mosquito breeding sites, thus lowering the population densities of malaria vectors. Personal protection includes measures that prevent contact between man and mosquitoes, such as ITN [12], IRS, window, and door screens. Although the use of ITN alone has been shown to reduce malaria morbidity and mortality [13,14], there is no doubt that better results will be achieved when combined with the indoor insecticide spray.
In addition to ITN, Roll Back Malaria (RBM) partnership recommends the use of intermittent preventive treatment (IPT) in areas of stable malaria transmission as a way of reducing the burden of this disease among pregnant women [15,16]. IPT consists of administration of curative dose of an effective anti-malarial drug at least twice during the second and third trimesters of pregnancy during routinely scheduled antenatal clinic visits regardless of whether the woman is infected or not [17,18]. The drug is administered under supervision during antenatal care visits. Sulfadoxine-pyrimethamine (SP) is the drug currently recommended for the IPT strategy [15,19]. Nigeria adopted this strategy in 2005. The current National Malaria Treatment Guideline and Policy in Nigeria recommends SP as first line agent for IPT and quinine for treatment of clinical malaria in all trimesters, Artemisinin-based combination therapy (ACT) is considered safe second line agents in the second and third trimesters [16,20] and may be used in the first trimester where there are no suitable alternatives [20]. WHO expects 80% of all pregnant women living in areas of high transmission to receive at least 2 doses of IPT during pregnancy by 2010 [21].
Kenya was one of the first countries to implement IPT, but the national coverage with 2 doses of SP was only 4% at 5 years after implementation [22]. Compliance in Tanzania too was very low, and this has been linked to poor acceptance of SP because of perceived association with side effects [23]. In a recent study to find out the knowledge and utilization of IPT among pregnant women attending antenatal clinics in primary health care centers in rural southwest, Nigeria, only 27.3% had received a dose of SP during the index pregnancy. The probable reason for the low uptake is the low level of awareness and poor knowledge of IPT by the pregnant women [24].
Indoor residual spray (IRS) is not yet adopted by the National Malaria Control Policy in Nigeria [25], and the government is practically doing nothing to encourage the use of indoor insecticide spray when compared to the amount of human and material resources devoted to ITN and IPT. With this singular loophole IMM cannot be said to be a policy in Nigeria, especially not in pregnant women. Therefore, this study was carried out to evaluate the most common mosquito control measures employed by the pregnant women as well as their effects on malaria infection. The use of IPT with SP was also evaluated.
MATERIALS AND METHODS
Study area
The study was conducted at Lagos Island Maternity Hospital, Lagos Nigeria. Lagos is situated in the southwestern part of Nigeria, an area of tropical rain forest with warm and humid climate where malaria transmission occurs all year round, like any other southern part of the country [25].
Ethical issues
Approval for the study was granted by the Lagos State Ministry of Health. Written informed consent was obtained from the participants. The questionnaires were administered by trained interviewers who interpreted the contents and the consent forms to those with poor understanding of English in local dialects. Those below the age of 18 years had their accompanying husband or older relatives consent for them.
Study population
The study was carried out over a period of 6 months between July and December 2009. All the pregnant women that consented to participate in the study during this period (n=400) were interviewed for the study. Women who were sick of malaria or any other form of illness were excluded from the study. Those who have taken antimalarial drugs within the last 4 weeks were also excluded. Questionnaires were administered to the participants so as to obtain information about their socio-demographic characteristics, ITN usage, IPT usage, and pregnancy history.
Evaluation of malaria prevention measures
The questionnaires elicited information about the usual mosquito control method adopted by participants and which has also been used in the previous night. They were also specifically questioned about the number of doses of IPT that has been taken under the supervision of health care workers during the antenatal visits had so far.
Sample collection
About 2 ml of venous blood was collected from the participants into EDTA bottles for malaria microscopy as well as for 3 MM Whatman filter paper blood spots.
Diagnosis of malaria
By antigen detection: SD BIOLINE Malaria Antigen P. falciparum (Korea), a malaria rapid diagnostic test kit (RDT) that detects histidin-rich protein-2 (HRP-2) specific for P. falciparum was used to initially screen the pregnant women at the point of sample collection.
By microscopy: Thick and thin Giemsa-stained blood smears were examined for malaria parasites at Nigeria Institute of Medical Research (NIMR) by accredited laboratory scientists, using standard methods [26,27]. The parasite density was determined in the thick film by counting the number of parasites against 200 leucocytes assuming the total leucocytes count to be 8,000 leucocytes/µl of blood. Parasite density was expressed as number of parasites per µl of blood. The thin film was used to verify the parasite specie. The hemoglobin (Hb) concentration of the women was also measured.
By species specific PCR for P. falciparum small subunit rRNA: Filter paper blots were transported from Nigeria to Germany where DNA was extracted using Tris-EDTA buffer-based extraction method [28], which yielded 100 µl of DNA in buffer. Nested PCR was carried out with primers described by Snounou et al. [29].Two genus-specific primers for Plasmodium spp. [-rPLU5-, (CCTGTTGTTGCCTTAAACTTC) and -rPLU6-, (TTAAAATTGTTGCAGTTAAAACG)] were used for the first cycle of amplification. P. falciparum species was detected using species-specific primers [-rFAL1-, (TTAAACTGGTTTGGGAAAACCAAATATATT) and -rFAL2-, (ACACAATGAACTCAATCATGACTACCCGTC)] in the second cycle (nested) reaction. The PCR assays were performed using the Peltier Thermal Cycler (PTC-0225) DNA Engine Tetrad (MJ Research inc., Walthan, Massachusetts, USA).
The thermal profile was 95℃ for 1 min (5 min at cycle 1), 60℃ for 2 min and 72℃ for 2 min for 45 cycles. A volume of 1 µl of the primary PCR product was used in the nested PCR reaction for 30 cycles. In both the first and nested PCR, reaction volume was 25 µl. The final concentration of each reagent was 1× PCR reaction buffer (10× PCR buffer-MgCl2), 1.5 mM MgCl2, 125 µM dNTP, 250 nM primers and 0.02 U/µl Taq Polymerase (QIAGEN, Hilden, Germany). PCR products (1,100 bp and 205 bp, respectively) were visualized by gel electrophoresis and ethidium staining.
Statistical methods
Analysis was performed using freely available GraphPad Instat 3.06 (San Digeo, California, USA). Non-parametric chi-square test was performed to evaluate the relationship between presence and absence of malaria in relation to the observed characteristics. Two-sided P-values of <0.05 indicate statistical significance.
RESULTS
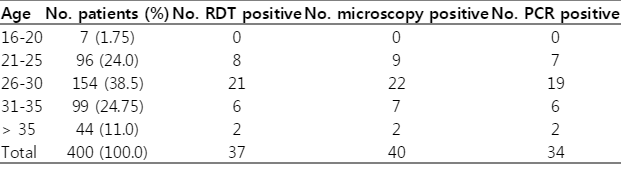
The overview of the laboratory results is presented in Table 1. The prevalence of infection with P. falciparum is dependent on the method used. Using microscopy, we detected a prevalence of 10%. Using the antigen test we got a prevalence of 9.3% and with P. falciparum-specific nested PCR, the prevalence reached 8.5%. We have to keep in mind that the 2 latter methods detected only P. falciparum. Because of its high sensitivity and specificity, PCR result was regarded as the true prevalence of infection.
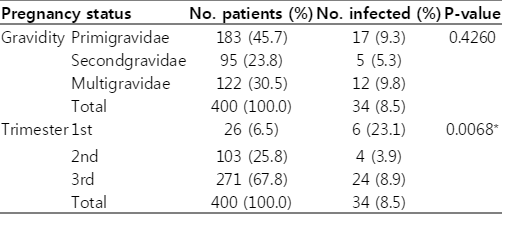
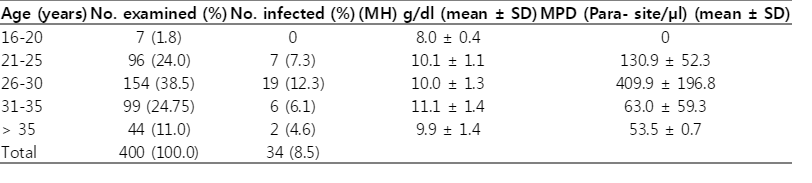
The age distribution, level of education, and the occupation pattern of the pregnant women are presented in Table 2. Out of the 400 pregnant women involved in the study, their majority were in the age range of 26 to 30 years (38.5%). The overall prevalence of the infection in the study population was 8.5%. The majority of the pregnant women were educated to the secondary and tertiary level (42.8% and 43.5%, respectively). Most of the participants were artisans (21.8%) and civil servants (21.8%), but malaria was most prevalent among the professionals (14.6%) and traders (14.0%). The secondgravidae had the lowest prevalence of malaria (5.3%) while the multigravidae had the highest (9.8%) (P=0.426). Most of the women were in their 3rd trimester (67.8%) with infection rate of 8.9%. The prevalence of malaria was the highest among the primigravidae (23.1%) (P=0.0068) (Table 3). Women within the age range of 16-20 years had the lowest mean hemoglobin concentration (8.0 g/dl) even though none of them was found with parasitemia. This was followed by the women older than 35 years (9.9 g/dl). Women within the age range of 26-30 years had the highest mean parasite density of 409.9/µl of blood, this was followed by those in the age range of 21-25 years with 130.9/µl (Table 4).
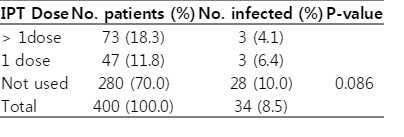
The most common malaria preventive measure was the use of insecticide spray (32.8%) , followed by the use of mosquito coil (27.5%). Only 15.5% depended on the use of ITN as the major mosquito control measure. The highest prevalence of infection was found among those who slept under an untreated net as the major control measure (28.0%). The infection rate was the lowest among those that used insecticide spray (2.3%), followed by those who employed the use of ITN (3.2%) to control mosquitoes (P=0.0001) (Table 5). Only 18.3% of the women have taken more than one dose of IPT during the index pregnancy, while 11.8% had taken only one dose. Yet, 70% were to take IPT. The prevalence of infection among the 3 groups was 4.1%, 6.4%, and 10.0%, respectively (P=0.086) (Table 6).
DISCUSSION
The prevalence of malaria in this study was 8.5%, this was largely different from previous studies in Lagos [5] and Osogbo [4], both in south-west Nigeria where the prevalence was between 60% and 72%, respectively. One reason for this large gap might be due to the diagnostic methods used. The overdiagnosis of malaria by microscopy must have occurred in previous studies. In this regard, overdiagnosis of malaria is not uncommon in endemic areas, for instance at 10 Tanzanian hospitals, 39% of 'positive' malaria slides were false positives and at 17 Kenyan outpatient clinics, the positive predictive value of a 'positive' slide was only 22% (negative predictive value, 93%) when compared to expert microscopy [30,31]. To exclude overdiagnosis of malaria, we used 3 different methods to detect parasitemia in the respective blood samples. Since nested PCR is the most specific and sensitive method, we relied on PCR results. Quite recently, the group around Agomo as well found a prevalence of 7.7% in a similar population in Lagos, Nigeria [32]. Furthermore, we only focused on P. falciparum which is the most import cause of malaria in Nigeria.
This study showed that there was no significant association between gravidity and prevalence of malaria, though prevalence was highest in the multigravidae (9.9%). This disagreed with the study in Lagos where the highest prevalence of infection (9.1%) was found among the primigravidae [32].
Though the majority of women in this study were in their 3rd trimester (67.8%), 6 of the 26 women in their 1st trimester were found to be positive with malaria parasites, this agrees with the general belief that malaria in pregnancy is commonest in the 1st trimester [33].
The mean hemoglobin concentration of the women were generally low (8.0 to 11.1 g/dl). Women of age range 16-20 years had the lowest level of hemoglobin (8.0 g/dl), paradoxically, none of them was positive for malaria parasite. This suggested that other factors were contributory to anemia in these women. This agreed with the WHO position that more than half of the pregnant women in the world are anemic with hemoglobin levels below 11 g/dl [34]. Similar results were seen among pregnant women in Abeokuta, Nigeria, which showed that 76.5% of the women investigated were anemic at 1 trimester of pregnancy or another, late registration for antenatal care was said to be the major reason behind this [35]. Systematic approach should be used to investigate the causes of anemia in pregnancy in this population, so that effective control measures can be put in place. The parasite density (mean and SD) was the highest among the women in the age group 26-30 years (409.9±196.80) who incidentally also had the highest prevalence of infection. It was the lowest in women who were over the age of 35 years (53.5±0.71).
The rate of ITN use in this study was low (15.5%). However, it showed an improvement in the rate of ITN usage among pregnant women in Nigeria, which was 4.4% in 2004 [6]. This may not be unconnected with increased funding of malaria control programs in the country within this period [25]. Insecticide spray was the commonest means of mosquito control in this study with the users having the lowest malaria infection rate (2.3%). The infection rate was also low among those that depended on ITN as the major malaria control method (3.3%). The malaria infection rate was the highest among the women that used untreated bed nets as the major control method (28.0%). There was a significant association between malaria infection and the major control method adopted by the pregnant women (P=0.0001). Only 18.3% of the women had taken more than one dose of IPT, while another 11.8% had taken a single dose, and the infection rate among them was 4.1% and 6.4%, respectively. The malaria prevalence was the highest among those who have not received any dose of IPT (10%). This finding was consistent with reports from Ibadan and other African countries which found IPT with SP to be protective against malaria in pregnancy [17,36,37].
This study focused on mosquito control measures that were mostly practiced by the study population; it was possible that adjunct control measures existed that were occasionally employed and may also contributed to the observed parasitemia recorded in this investigation. Further studies may be designed to investigate this, and even to follow-up the women from the day of booking to the date of delivery so as to document the outcome of IPT and ITN on delivery.
In summary, our study showed that though use of insecticide spray is not a policy in Nigeria, it is equally an effective malaria control strategy, and if properly implemented, it will impact positively on malaria control in Nigeria, especially if residual insecticides are deployed. The basic recommendation of a sustained integrated mosquito management which requires alternative use of different classes of insecticides, in conjunction with resistance monitoring, source reduction, biological control, and public education [38] should be strengthened in Nigeria.
ACKNOWLEDGMENTS
We acknowledge Deutscher Akademischer Austausch Dienst (DAAD) for providing sponsorship for the bench work in Germany, Professor Dr. M. Lanzer, Department of Infectiology and Parasitology, University of Heidelberg, Germany who provided P. falciparum Dd-2 and HB-3 reference strains for the PCR. Appreciation is extended to Dr. Olusola Ojuronbge, Institute of Tropical Medicine, Tuebingen, Germany and to Dr. Ibukun Aibinu, Otto Von Guericke University, Magdeburg, Germany for technical assistances.