Peripheral gangrene in patients with severe falciparum malaria: report of 3 cases
Article information
Abstract
Peripheral gangrene, characterized by distal ischemia of the extremities, is a rare complication in patients with falciparum malaria. Patients with this complication have generally undergone early amputation of the affected areas. In this report, we describe 3 adult Thai patients presented at the Hospital for Tropical Diseases, Bangkok, with high grade of fever ranged 6-9 days, jaundice, acute renal failure, respiratory failure, alteration of consciousness and shock. Two patients had gangrene developed at the lower extremities on day 1 of hospitalization and 1 patient had gangrene developed on day 3. Blood smears revealed hyperparasitemia with Plasmodium falciparum. These patients were diagnosed as having severe malaria with peripheral gangrene. The resolution of gangrene was successfully achieved by treatment with artesunate and conservative treatment in 2 of 3 cases.
INTRODUCTION
The microcirculation is compromised in Plasmodium falciparum malaria as a result of the adhesion of infected erythrocytes to vascular endothelium. Symmetrical peripheral gangrene is characterized by distal ischemic damage in 2 or more extremities, without large vessel obstruction. This syndrome has been reported in several conditions such as infections, disseminated intravascular coagulation (DIC), low cardiac output states, and rarely associated with falciparum malaria (Alexander et al., 1975; Mohantly et al., 1985; Chittichai et al., 1991; Hayes et al., 1992; Kochar et al., 1998; Davis et al., 2001; Sharma and Gupta, 2002; Liechti et al., 2003). We report 3 cases of severe falciparum malaria with peripheral gangrene and their treatments.
CASE REPORTS
Case 1
A 40-year-old Thai man gave a 6-day history of high fever with chills, headache, anorexia, nausea and vomiting. Five days later, he became drowsy and short of breath. On the sixth day, he was transferred to the Hospital for Tropical Diseases, Bangkok, where he developed a generalized tonic clonic seizure that lasted for 5 minutes. There was no history of any underlying disease, alcohol consumption, or smoking.
On physical examination, the temperature was 40.8℃, pulse rate 142/min, blood pressure 109/67 mmHg and respiratory rate 28/min. He was dyspneic with marked icteric sclera, dysconjugate gaze and stupor with a Glasgow coma scale of 8. He required ventilator support, isotonic saline and inotropic therapy (dopamine) to maintain arterial blood pressure. Cardiopulmonary examination revealed tachycardia and tachypnea, but was otherwise normal. The liver and spleen were not palpable. Diffuse purpuric patches were noted in the lower extremities together with gangrene involving large areas of the skin. The toes were cyanotic and became dark blue 24 hr after admission (Fig. 1). The posterior tibial and dorsalis pedis arterial pulses were normal.
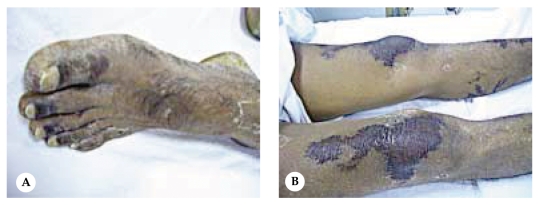
Gangrene involving the toes of left foot and large skin areas of lower extremities on day 14 of hospitalization (Case 1). A: left foot, B: extensor surface of both knees.
The peripheral blood smear revealed 207 ring forms and 4 gametocytes of Plasmodium falciparum per 1,000 red cells, anemia (hemoglobin 9.7 g/dl) and normal platelet counts (395,000/mm3). Blood chemistry revealed a slightly low blood glucose level (72 mg/dl) and signs of renal failure (blood urea nitrogen 64.5 mg/dl, creatinine 8.12 mg/dl). He had cholestatic jaundice (total bilirubin 2.65 mg/dl, direct bilirubin 1.6 mg/dl). Radiography of the chest was normal.
The patient was treated with intravenous artesunate (total dose 1,200 mg), and underwent hemodialysis for renal failure. Dopamine was reduced and discontinued after 4 days of hospitalization. Parasites disappeared from the peripheral blood smear after 11 days of treatment. Hemodialysis was discontinued after 2 months of hospitalization when renal function had fully recovered. There was complete resolution of the gangrene in his lower extremities at the end of 3 months.
Case 2
A 45-year-old Thai man was admitted to the Intensive Care Unit of the Hospital for Tropical Diseases, Bangkok, with a history of high fever, chills, abdominal pain and myalgia for 9 days, and confusion for 24 hr prior to admission. He had no history of any underlying disease, excessive alcohol consumption, or smoking.
On physical examination, his temperature was 39.2℃, pulse rate 120/min, blood pressure 110/70 mmHg and respiratory rate 36/min with abnormal abdominal reflexes. He had markedly icteric sclera, a dysconjugate gaze, and coma with a Glasgow coma scale score of 3. Cardiopulmonary examination revealed tachycardia and rhonchi in both lungs. The liver was 12 cm in span, soft and non-tender. Examination of the lower extremities revealed livido reticularis. Ventilator support was initiated because of respiratory failure. The blood pressure dropped after intubation, so the patient was resuscitated with normal saline, human albumin and inotropic drugs (dopamine and adrenaline) to maintain arterial blood pressure. He underwent hemodialysis for renal failure and severe acidosis.
The peripheral blood smear revealed 197 ring forms and 7 gametocytes of P. falciparum per 1,000 red cells, normal hemoglobin (12.3 g/dl), leukocytosis (12,600/mm3) with 15% band forms and thrombocytopenia (platelets count 23,000/mm3). The prothrombin time was prolonged to 45 seconds. Blood chemistry revealed normal blood glucose level (92 mg/dl), renal failure (blood urea nitrogen 93 mg/dl, creatinine 4.2 mg/dl), severe metabolic acidosis (serum bicarbonate 15 mmol/l, arterial blood pH 7.160), and cholesteato-hepatitis (total bilirubin 19.8 mg/dl, direct bilirubin 15.58 mg/dl, SGOT 340 U/L, SGPT 230 U/L). Radiography of the chest was normal.
The patient received 1,200 mg of artesunate and 750 mg of mefloquine and the parasites were clear from the peripheral blood smear after 9 days of admission. On the third day of hospitalization, his toes on both feet became bluish-purple, and progressed to dry gangrene over the ensuring 2 weeks (Fig. 2). The posterior tibial and dorsalis pedis arterial pulsations were normal. The dosage of adrenaline and dopamine were progressively reduced and discontinued after 12 days. He also received hemodialysis for 6 weeks. He was referred to a surgeon for amputation of 5 fingers of his right foot after 8 weeks of hospitalization. The patient fully recovered consciousness as well as liver and renal function after 3 months of illness.
Case 3
A 59-year-old Thai woman developed high fever, chills and rigors for 6 days. She also had shortness of breath, oliguria and alteration of consciousness for 24 hr prior to hospitalization. There was no history of underlying diseases.
On physical examination; the temperature was 38.3℃, pulse rate 155/min, blood pressure 77/58 mmHg and respiratory rate 28/min. She was comatose with a Glasgow coma scale rating of 3 and a dysconjugate gaze. She had marked icteric sclera and was moderately pale. Physical examination of the heart and lungs revealed marked tachycardia, but was otherwise normal. The liver and spleen were not palpable. Examination of the toes revealed a bluish purple discoloration. The posterior tibial and dorsalis pedis arterial pulsations were normal. She was resuscitated with isotonic saline, human albumin and given ventilator support. Dopamine and norepinephrine (levophed™) were adjusted in order to maintain an adequate arterial blood pressure.
The peripheral blood smear revealed 102 ring forms and 3 gametocytes of Plasmodium falciparum per 1,000 red cells anemia (hemoglobin 10 g/dl), leukocytosis (16,300 /mm3) with 17% band forms and thrombocytopenia (platelets count 34,000/ mm3). Blood chemistry revealed increased blood glucose level (192 mg/dl), renal failure (blood urea nitrogen 52 mg/dl, creatinine 3.9 mg/dl), cholesteato-hepatitis (total bilirubin 16.7 mg/dl, direct bilirubin 12.59 mg/dl, SGOT 597 U/L, SGPT 290 U/L). Radiography of the chest was normal.
The patient received 1,200 mg of artesunate, 750 mg of mefloquine and hemodialysis for 2 weeks. The dopamine and levophed™ were discontinued after 3 days of admission. On day 2, her toes became well perfused with complete resolution of the ischemia. The patient had an uneventful recovery.
DISCUSSION
Symmetrical peripheral gangrene is an uncommon complication of falciparum malaria reported mainly in Asian countries. The exact pathogenesis for bilateral gangrene remains uncertain and may be multifactoral. As presented in Table 1, most of the cases reported in the literature were associated with DIC (Mohantly et al., 1985; Chittichai et al., 1991; Kochar et al., 1998; Sharma et al., 2002; Liechti et al., 2003). Infected red cells may play an important role in initiating protocoagulant activity or the indirect effects of clotting cascade activation may lead to the blockage of small capillaries and DIC (Clemens et al., 1994;Mohanty et al., 1997; Levi and Ten Cate, 1999). The presence of tight packing of the parasitized erythrocytes by decreased deformability of red cells or adherence of infected red cells to microvascular endothelium will initiate a microcirculatory obstruction (Macpherson et al., 1985).
The 3 patients described in this report exhibited many clinical similarities. They were all heavily parasitized enough to develop cerebral malaria, acute renal failure, and shock. Full laboratory tests for DIC were not performed, but 2 patients had persistent thrombocytopenia. Thus, they might have had some degree of DIC. In the first and third patient, ischemic toes were noted at the time of admission, while the second patient had peripheral gangrene after 3 days of treatment. The resolution of the ischemia was complete in the first and third patients with no surgical intervention. In all 3 cases the symmetrical peripheral gangrene developed in association with vasopressors, DIC and/or malarial infection.
From the study of Edwards (1980) the early management of this condition with heparin or streptokinase was successful. However, bleeding is a complication from anticoagulant therapy, so the patients should have careful monitoring of all clotting factors, and platelet concentrations should be given as soon as they are indicated (Edwards, 1980; Levi and ten Cate, 1999). The resolution of the gangrene in 2 of the 3 patients in this report suggests an initially conservative approach to the management of symmetrical peripheral gangrene. This allows time for the patient's condition to stabilize and allows the gangrenous lesions to become completely recovered.

