Two human cases of tick bite caused by Ixodes nipponensis
Article information
Abstract
We report two human cases of tick bite. A 63-year-old male had a pruritic pea-sized brownish nodule on the left popliteal area. Another 41-year-old male had an asymptomatic bean-sized black nodule in the pubic area. The ticks were identified as Ixodes nipponensis, which are the 18th and the 19th cases in Korea.
Ticks (Ixodidae) are one of the blood-sucking arthropods, that is distributed worldwide. Its natural hosts are wild animals, but it also attacks and feeds on man and domestic animals (Marshall, 1967). Tick bites not only induce a variety of skin lesions but also transmit viral, rickettsial, bacterial, and protozoal diseases (Marshall, 1967; Wilson and King, 1999), which were considered to be very important in public health care. In addition, ticks, particularly the genus Ixodes, are the major vector for Borrelia burgdorferi infection. Lyme disease caused by B. burgdorferi was reported in Korea (Park et al., 1992; Lee et al., 1993). Therefore, it is necessary to rule out borreliosis in humans with tick bite. The severity of the skin reaction to tick bite may depend on several factors, such as duration of feeding, size of the mouth part, type of tick secretion, previous exposure to the tick or related species, and allergic reaction of the host (Marshall, 1967; Cho et al., 1994; Wilson and King, 1999).
Case 1
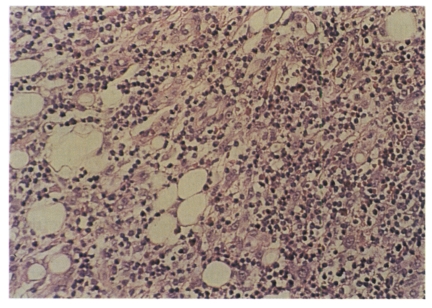
A 63-year-old male with a pruritic pea-sized brownish nodule in the left popliteal area was referred to us in June 1999. Asymptomatic solitary nodule had been found in the left popliteal area about 20 days before admission. Then, the nodule was accompanied by pruritus, erythema, and pain. He was a farmer and frequently worked in the field. Past history and family history were nonspecific. On admission, the erythematous area was surmounted by a 5×7 mm sized arthropod which was firmly attached to the skin by the mouth part (Fig. 1). Laboratory studies were normal or negative. The tick and surrounding skin were removed intact by an excision biopsy, and submitted for histologic study. Histopathologic examination revealed dilated vessels and dense perivascular inflammatory infiltrates composed of lymphocytes and eosinophils in the dermis and subcutis (Fig. 2). After excision, the wound healed well and no recurrence happened.
Case 2
A 41-year-old male complained of an asymptomatic bean-sized black nodule in the pubic area, when he visited the dermatologic clinic in June 2001. At 2 weeks before admission, he climbed a mountain. After he came back home, he found an arthropod on the back and removed it by himself. He also felt a mildly anesthetic sensation in the pubic area 2 days later and found a black colored nodule. The nodule became bigger, therefore, he thought that it might be a tumor. Past history and family history were nonspecific. On admission, the nodule was a black arthropod, 7×8 mm in size, firmly attached to the skin by the mouth part (Fig. 3). It was easily removed by heat, and all signs and symptoms disappeared.

A bean-sized tick was firmly attached on the skin of pubic region in the case 2. The tick was engorged with blood meal.
The tick from the case 1 was oval in shape, 5×7 mm in size, and light brown in color (Fig. 4A and 4B). Another tick from the case 2 was oval, 7×8 mm in size, and black in color (Fig. 5). The capitulum of anterior portion of the body, the scutum of dorsal portion, spicular plate, genital aperture, anus, and 4 pairs of legs of ventral portion were observed. Spicular plate was ovoid and located on the ventrolateral surface posterior to the coxa IV. Genital opening was straight and located on the level of the coxa IV. Anus was round and located on the posterior portion, and horseshoe-shaped anal groove was extended to posterior margin of the body, surrounding the anus (Fig. 5). Internal spur of the coxa I was long, but not overlaid on the edge of the coxa II in the case 1 (Fig. 6A) and the case 2 (Fig. 6B). These characteristics were typical features of I. nipponesis (Lee et al., 1989; Cho et al., 1995; Ryu et al., 1998).
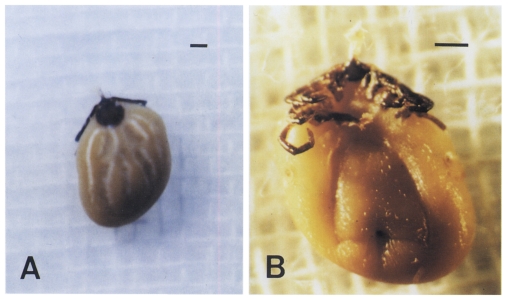
Ixodes nipponensis after removal with dorsal view (A) and ventral view (B) in the case 1. Scale bars = 1 mm.
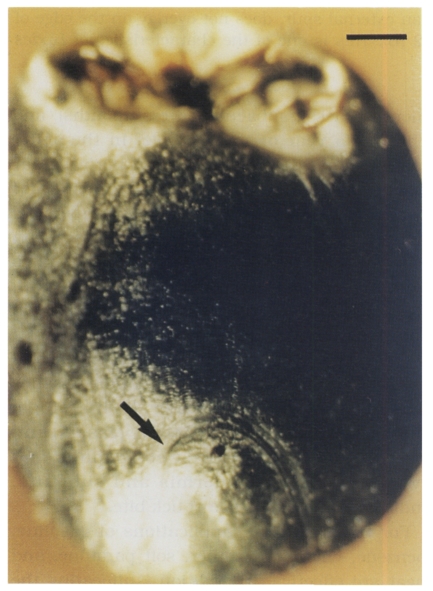
The tick removed from pubic area in the case 2. The whole body with ventral view. Inverted U-shaped anal groove (arrow) encircles the anus. A scale bar = 1 mm.
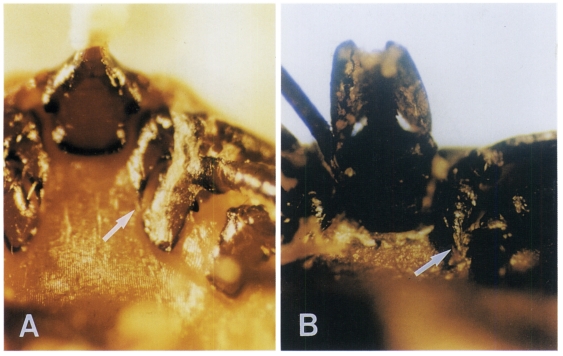
Internal spur (arrow) of coxa I, much longer than external spur, does not overlay on the edge of coxa II in the ticks from the case 1 (A) and the case 2 (B). This is one of the characteristics of Ixodes nipponensis.
Thirty-one cases of tick bite have been reported in Korea up to the present (Yun et al., 2001). Seventeen cases were identified with I. nipponensis (Noh and Cho, 1983; Lee et al., 1989; Paik et al., 1989; Chang et al., 1991; Cho et al., 1991; Cho et al., 1994, 1995; Chu et al., 1997; Ryu et al., 1998; Chae et al., 2000; Yun et al., 2001), and 1 case with I. ovatus (Chang et al., 1991), 1 case with I. monospinosus (Cho et al., 1999), 1 case with I. persulcatus (Im et al., 1998), 1 case with Haemaphysalis flava (Yoon et al., 1996), and 1 case with Haemaphysalis longicornis (Rho et al., 1999) have been reported. The remainder were with Ixodes as the genus level. Our cases are the 18th and the 19th cases with I. nipponensis.
Ticks are usually 1-9 mm long before engorgement, but they reach 2 cm in length after feeding (Marshall, 1967). Ticks feed for 7-12 days for a full engorgement and then drop off the hosts to continue their life cycle (Wilson and King, 1999; Odom et al., 2000; Yun et al., 2001). Some ticks may feed for 30 days or longer (Yoon et al., 1996; Chu et al., 1997). The case 1 fed over 20 days and the case 2 for 14 days. During this time, the patients suffered from fever, chill, headache, abdominal pain, and vomiting. After removal of the engorged ticks, the above symptoms disappeared within 12 to 36 hours (Odom et al., 2000).
The most frequent location of tick bites is known to be perianal area, abdomen, scrotum, extremities, and scalp (Cho et al., 1994; Yun et al., 2001). In our cases, the locations were on the leg and the pubic area. Tick bites occur mostly in the spring and summer. Our cases were detected in June.
Dermatoses by the tick bite include papular urticaria, subcutaneous hemorrhage, focal necrosis, peladoid alopecia, secondary bacterial infection, erythema chronicum migrans, acrodermatitis chronica atrophicans, and lymphocytoma cutis. Neurologic manifestations due to tick saliva are pyrexia and paralysis (Marshall, 1967; Patterson et al., 1979). Our case 2 patient felt mild anesthesia in the pubic lesion. Due to very slow penetration of the skin by the insect's hypostome and the fact that the insect's saliva is both anticoagulant and anesthetic, the patient hardly feels pain or itching sensation and it may take several days to find the tick on the body surface (Winer and Strakosch, 1941).
Winer and Strakosch (1941) divided the histological findings of tick bite into three stages with reference to duration: acute (a month or less), subacute (several months), and chronic (a year or more) stage. In the acute stage, dilated blood vessels and perivascular inflammatory infilitrates composed of lymphocytes and eosinophils in the superficial dermis are observed. In the subacute stage, extensive perivascular inflammatory infilitrates composed of lymphocytes, neutrophils, fibroblasts, and eosinophils are prominent. In the chronic stage, fibrous tissue proliferation, a few Langhans' giant cells, lymphocytes, and eosinophils deposited between fibrous tissues are observed. In the case 1, histologic manifestations were dilated vessels and perivascular infiltrates of eosinophils and lymphocytes in the dermis and subcutis, indicating an acute stage of tick bite.
For the treatment, applications of gasoline, benzene, chloroform, ether, soft paraffine, and heat are effective. In addition, suffocating the tick with petrolatum is recommended. Abrupt pulling or squeezing of the tick is discouraged, because mouth part may be left behind the skin and secretion of salivary toxins may be increased to aggravate inflammation or foreign body reaction. For this reason, punch biopsy or surgical excision is very effective, particularly when the tenacious tick cannot be easily extracted by other means (Winer and Strakosch, 1941; Patterson et al., 1979; Cho et al., 1994; Wilson and King, 1999). In our cases, we removed ticks by excision biopsy and heat to prevent saliva release and transmission of any microorganism during tick manipulation. Regular follow-up was carried out, but no recurrence or other disorder was observed.