A Case of Post Kala-Azar Dermal Leishmaniasis in India
Article information
Abstract
Post kala-azar dermal leishmaniasis (PKDL) is a rare disease. This is a solitary case report from Orissa, India. We describe a case of PKDL in a 55-year-old male who presented with multiple nodular lesions over face, trunk, and extremities. The patient had been to an endemic area of kala-azar and had a previous history of leishmaniasis. Fine needle aspiration cytology samples from skin nodules revealed Leishmania amastigotes.
INTRODUCTION
Post kala-azar dermal leishmaniasis (PKDL) accounts for about 5-10% of visceral leishmaniasis in India [1]. Both PKDL and VL are caused by Leishmania amastogotes, which are the commonest causative organism for kala-azar in India. PKDL is seen in about 10% of kala-azar patients in our country [2]. This is the first reported case of PKDL from Orissa, India to the best of our knowledge.
CASE REPORT
A 55-year-old male farmer of Orissa, India developed a whitish depigmented macule over trunk, clinically diagnosed as tuberculoid leprosy and was under treatment in a rural dispensary. Within 5 months, the macule gradually developed into erythematous patches followed by multiple non-ulcerated, soft, and painless cutaneous nodules all over the face, trunk, and extremities (Fig. 1). No mucosal involvement was seen.
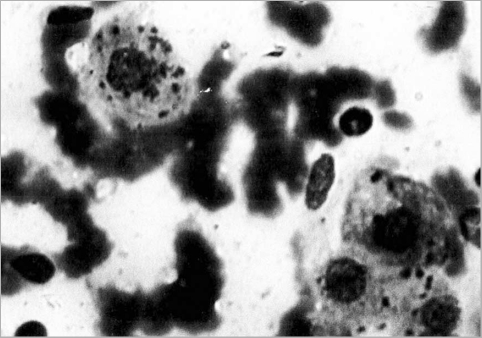
The patient was sent for fine needle aspiration cytology (FNAC) of skin nodules. The aspiration smears stained with May Grunwald Giemsa (MGG) revealed plenty of Leishmania amastogotes inside the histiocytes along with few in the background (Fig. 2). Special stains like periodic acid-Schiff (PAS) and acid-fast bacillus (AFB) were done as advised by the clinicians to rule out the possibility of lupus vulgaris and fungal infection. Both the stains were negative. On close questioning the patient revealed having been to Bihar 3 years back where he had taken sodium antimony gluconate (SAG) therapy for VL. Clinical history supported by cytology helped us in giving a diagnosis of cutaneous leishmaniasis (CL). Aspirations from the liver, spleen, and bone marrow were negative for parasites. Few basic investigations like blood sugar, venereal disease research laboratory (VDRL) test, test for human immunodeficiency virus (HIV), and ultrasonography were advised to the patient, which revealed no abnormality. The patient is responding well to SAG therapy and most of the lesions disappeared.
DISCUSSION
CL is a dermatological disease known since earliest antiquity, and reported at the end of the 19th century to be caused by a parasite protozoan. CL presents as a skin lesion, which are generally localized, without involvement of the mucosa, and not a generalized infection [3,4]. Rarely, dermotropic parasites may give rise to diffused cutaneous leishmaniasis (DCL). Clinically the nodules may be localized or diffused involving the whole body. Recidivans leishmaniasis is another minor localized form of CL. Diffused form may be associated with HIV infection. Our case was not associated with HIV infection.
We report this case from Orissa, India where the lesions were purely cutaneous. In our case, the patient had a previous treated history of kala-azar about 3 years back. PKDL generally appears within 2-10 years of treated VL. In a case reported by Mittal et al. [5] the incubation period was more than 10 years.
Diagnosis of PKDL can be done from clinical history supported by rapid and direct demonstration of Leishmania amastogotes in cytosmears or biopsies [6]. The organism is best revealed by Giemsa stain as reddish cytoplasmic, round to oval structures with a very small rod-like similarly stained projection (kinetoplasts). Culture with classical blood agar, Novy-MacNeal-Nicolle (NNN) medium, is a useful complement for parasitological diagnosis and drug sensitivity. Molecular diagnosis has been successfully applied to the diagnosis of CL. The detection of parasite DNA is achieved through PCR amplification. Some recent studies quote that high concentrations of IL-10 in the peripheral blood of non-treated VL patients and interferon-γ in the serum of treated VL patients predict the chances of future development of PKDL [1,7]. The above facts can be demonstrated by specialized tests like PCR and immunoblotting for anti-rK39 antibodies [7].
On reporting this case, we have highlighted the fact that PKDL, though uncommon, is a distinct manifestation of VL.