Abstract
Lupoid leishmaniasis is a unique form of cutaneous leishmaniasis characterized by unusual clinical features and a chronic relapsing course, mostly caused by infection with Leishmania tropica. In this clinical form, 1-2 yr after healing of the acute lesion, new papules and nodules appear at the margin of the remaining scar. Herein, we describe a case of this clinical form that was resistant to 2 courses of treatments: systemic glucantime and then a combination therapy with allopurinol and systemic glucantime. However, marked improvement was seen after a combination therapy with topical trichloroacetic acid solution (50%) and systemic glucantime, and there were no signs of recurrence after 1 yr of follow-up.
-
Key words: Leishmanis tropica, cutaneous leishmaniasis, trichloroacetic acid
INTRODUCTION
Leishmaniasis currently threatens 350 million people in 88 countries around the world. Up to 90% of cutaneous leishmaniasis (CL) cases occur in Afghanistan, Brazil, Iran, Peru, Saudi Arabia, and Syria. Lesions can be very disfiguring, particularly on the face, which may have long-term psychological and social consequences [
1]. Lupoid leishmaniasis is a clinical form that was described in 1923 [
2], and it is a chronic condition that typically follows acute cutaneous leishmaniasis infection. One to 2 yr after healing of the acute lesion, new papules and nodules will appear at the margin of the remaining scar [
3]. The papules have a glaucomatous appearance and are often scaly. Most reported cases were associated with old world strains of leishmaniasis rather than new world strains, and
Leishmania tropica was the responsible agent in their majority [
3]. The incidence of lupoid leishmaniasis reported in previous studies ranges from 0.5-6.2% [
4,
5].
Lupoid CL is prevalent in the endemic area of leishmaniasis, particularly in the Middle East and Afghanistan [
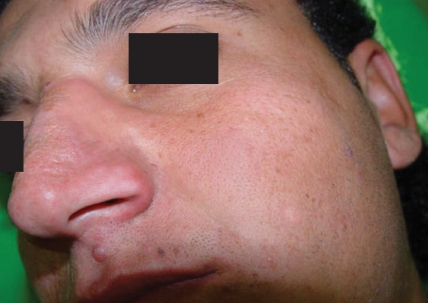
4]. Histological features of this condition include well-organized epithelioid granuloma surrounded by lymphocytes, the absence of amastigotes, and frequent negative cultures for leishmaniasis [
5]. However, the leishmanin test is usually positive [
6]. Herein, we describe a case of lupoid leishmaniasis that was resistant to systemic glucantime yet responded to a combination therapy with glucantime and topical application of trichloroacetic acid (TCA) solution.
CASE REPORT
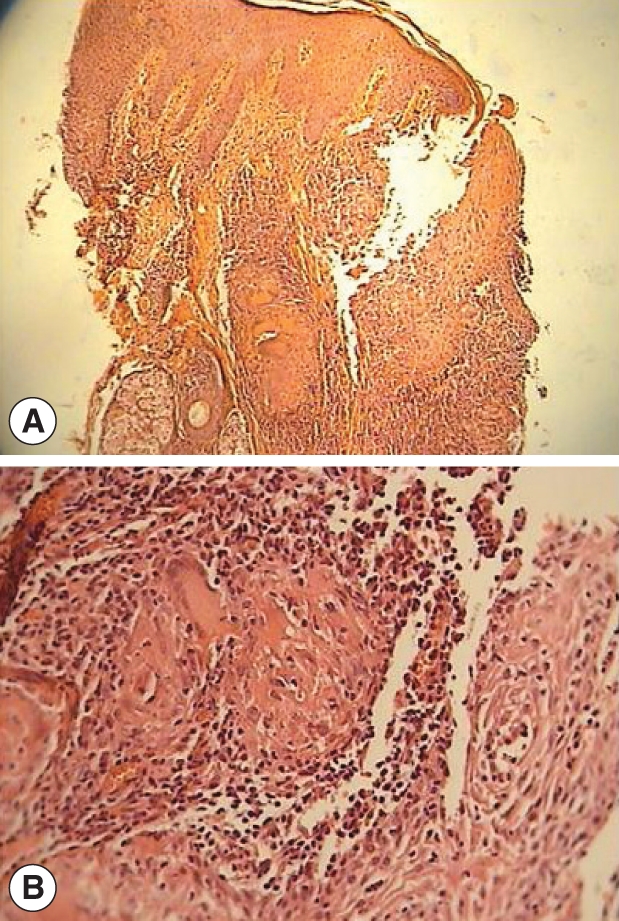
A 19-yr-old Afghan man presented with a large atrophic scar on the nose, and there were some red infiltrative nodules at the margin of the lesion present for the last 3 yr (
Fig. 1). At the beginning of the disease (3 yr ago), a direct smear was taken from the lesion and was positive for leishman bodies. The patient had been treated for CL with glucantime. The lesion improved, but it recurred after 1 yr. At the time of our visit, the patient's direct smear was negative for leishman bodies, and a histological examination indicated epidermal hyperplasia, severe infiltration of lymphoid plasma cells and epithelioid granuloma without caseous necrosis or leishman bodies, but the leishmanin test (Pasteur Institute, Tehran, Iran) was positive. The patient was treated with 2 courses of systemic glucantime (Aventis, Paris, France) at 20 mg/kg/day intramuscularly (IM) for 20 days and with a combination therapy of systemic glucantime (IM) at 20 mg/kg/day for 20 days plus allopurinol (Hakim, Tehran, Iran) at 20 mg/kg/day for 20 days, but relapse occurred after cessation of the treatment. We treated the patient with a combination therapy of topical TCA and systemic glucantime. After cleansing with alcohol, TCA (Merck, Berlin, Germany) (50% wt/vol) [
7] was applied to the lesion using a cotton swab, and after frosting, the lesion was covered with vaseline (
Fig. 2). There was no need to wash off any TCA from the lesion. TCA was applied once weekly for 3 wk. In addition, the patient was treated with systemic glucantime at 20 mg/kg/day for 20 days. The responses to the treatment were good, and the marginal nodules disappeared (
Fig. 3). The patient was followed-up for 1 yr and showed no signs of recurrence.
DISCUSSION
Clinically and histologically, lupoid leishmaniasis is similar to lupus vulgaris, which is the most important differential diagnostic consideration [
8]. Differential diagnosis is difficult and may depend on detection of
Leishmania amastigotes in the histological sections, growth of promastigotes in cultures, or identification of amastigotes by other techniques. This chronic condition typically follows acute CL, and in the majority of cases,
Leishmania tropica is the causative agent [
9].
There is no standard treatment for this condition, and multiple treatments have been reported with varying degrees of success [
10]. Treatment options include intraregional pentavalent antimony [
11], a combination therapy with intramuscular injection of meglumine antimoniate (MA) and allopurinol [
12], local injection of amphothericin B [
13], levamisole [
14], dapsone [
15], cryotherapy [
16], and triple therapy with paromomycin, cryotherapy, and intralesional meglumine antimoniate [
5].
In a previous study that was done in Isfahan, the efficacy of topical TCA (50%) in the treatment of CL was evaluated, and the response to the treatment was the same as the intraregional meglumine antimoniate [
17]. TCA peeling has been used for the treatment of several skin lesions, including actinic degeneration and acne scarring. Its efficacy could be due to epidermal regeneration as well as to the regeneration of new collagen in the dermis.
Our patient, who was resistant to 2 courses of treatment with systemic glucantime and a combination therapy with glucantime and allopurinol showed marked improvement after a combination therapy with topical TCA (50%) and systemic glucantime. Additionally, there was no recurrence after 1 yr of follow-up. The good efficacy of TCA in the treatment of the above condition could be due, in part, to enhancing macrophage activity in addition to epidermal and collagen regeneration. We suggest that, in a randomized clinical trial, the efficacy of this combination treatment would be evaluated against systemic glucantime for the treatment of lupoid CL.
References
Fig. 1Large atrophic scar (arrow) on the nose with red infiltrative nodules at the margin.

Fig. 2Pseudoepitheliomatous hyperplasia of epidermis with small tuberculoid granuloma and mild to moderate mononuclear cell infiltrates (A ×40; B ×100).
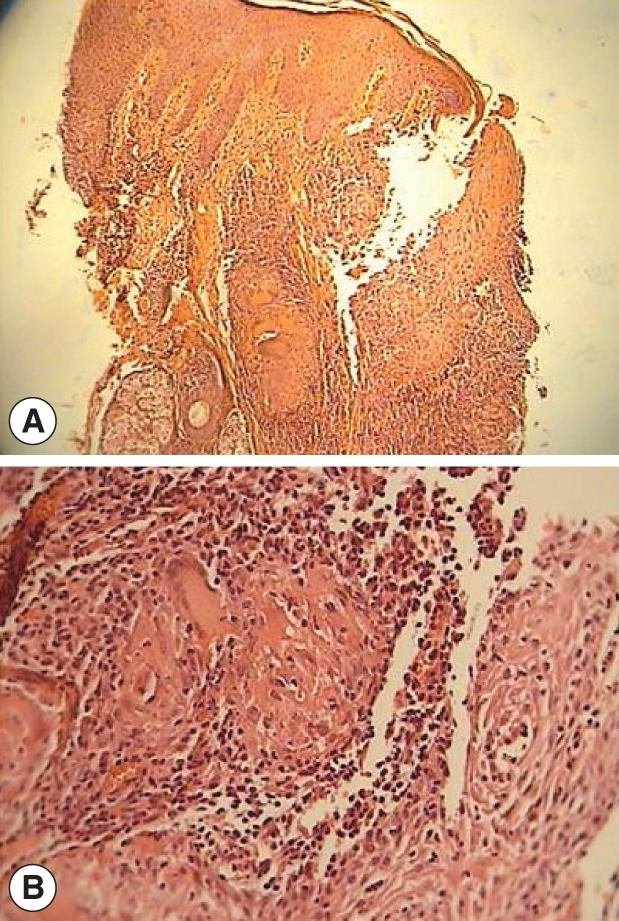
Fig. 3Frosting the lesion after application of 50% TCA solution.

Fig. 4The patients after 1 yr of follow-up showing complete healing of the lesion.

Citations
Citations to this article as recorded by

- A History of the Advances in Chemical Peeling in Dermatologic Surgery Since 2000
Haya Raef, Harold J. Brody, Gary D. Monheit, William P. Coleman
Dermatologic Surgery.2025; 51(9): 831. CrossRef - Atypical Manifestations of Old World Cutaneous Leishmaniasis: A Systematic Review and Clinical Atlas of Unusual Clinical and Specific Anatomical Presentations
Bahareh Abtahi‐Naeini, Seyed Naser Emadi, Zabihollah Shahmoradi, Mahsa Pourmahdi‐Boroujeni, Ali Saffaei, Fereshte Rastegarnasab
Health Science Reports.2025;[Epub] CrossRef - Old world cutaneous leishmaniasis in Iran: clinical variants and treatments
Alireza Firooz, Hossein Mortazavi, Ali Khamesipour, Maryam Ghiasi, Robabeh Abedini, Kamran Balighi, Nafiseh Esmaili, Mansour Nassiri-Kashani, S. Ebrahim Eskandari, Mehdi Mohebali, Akram Mir Amin Mohammadi, Yahya Dowlati
Journal of Dermatological Treatment.2021; 32(7): 673. CrossRef - Novel Strategies and Pharmaceutical Agents for the Treatment of Leishmaniasis: A Review
Mohammad A. Nilforoushzadeh, Maryam Heidari-Kharaji, Mehrak Zare, Elham Torkamaniha, Sima Rafati
Anti-Infective Agents.2020; 18(2): 89. CrossRef - Synergic Effect of Allopurinol in Combination with Nitroheterocyclic Compounds against Trypanosoma cruzi
Ana Lia Mazzeti, Lívia de F. Diniz, Karolina R. Gonçalves, Ruan Schott WonDollinger, Tassiane Assíria, Isabela Ribeiro, Maria T. Bahia
Antimicrobial Agents and Chemotherapy.2019;[Epub] CrossRef - Comparison of Lesion Improvement in Lupoid Leishmaniasis Patients with Two Treatment Approaches
Mahnaz Banihashemi, Mohamad Javad Yazdanpanah, Hossein Amirsolymani, Hadis Yousefzadeh
Journal of Cutaneous Medicine and Surgery.2015; 19(1): 35. CrossRef - Comparison Between Intralesional Meglumine Antimoniate and Combination of Trichloroacetic Acid 50% and Intralesional Meglumine Antimoniate in the Treatment of Acute Cutaneous Leishmaniasis: A Randomized Clinical Trial
Mohammad Ali Nilforoushzadeh, Fariba Jaffary, Roya Derakhshan, Elaheh Haftbaradaran
Journal of Skin and Stem Cell.2014;[Epub] CrossRef - Lupoid leishmaniasis of the nose responding well to cryotherapy
RYM BENMOUSLY MLIKA, HOUDA HAMMAMI, ASMA SIOUD, INçAF MOKHTAR, SAMY FENNICHE
Dermatologic Therapy.2011; 24(3): 378. CrossRef - Discoid chronic lupus erythematosus at the site of a previously healed cutaneous leishmaniasis: an example of isotopic response
F. Bardazzi, F. Giacomini, F. Savoia, C. Misciali, A. Patrizi
Dermatologic Therapy.2010; 23: S44. CrossRef