Abstract
In this study, we intended to describe a human case of lumbosacral canal sparganosis in People’s Republic of China (China). A 56-year-old man was admitted to Xiangya Hospital Central South University in Changsha, Hunan province, China after having an experience of perianal pain for a week. An enhancing mass, a tumor clinically suggested, was showed at the S1–S2 level of the lumbosacral spine by the examination of magnetic resonance imaging (MRI) with gadolinium contrast. The patient was received the laminectomy from S1 to S2, and an ivory-white living worm was detected in inferior margin of L5. In ELISA-test with cerebrospinal fluid (CSF) and serum samples, anti-sparganum antibodies were detected. He had a ingesting history of undercooked frog meat in his youth. By the present study, a human case of spinal sparganosis invaded in lumbosacral canal at the S1–S2 level was diagnosed in China. Although the surgical removal of larvae is known to be the best way of treatment for sparganosis, we administered the high-dosage of praziquantel, albendazole and dexamethasone to prevent the occurrence of another remain worms in this study.
-
Key words: Sparganosis, lumbosacral spine, sparganum, praziquantel
INTRODUCTION
Sparganosis is a neglected helminthic infection caused by invasion of the plerocercoid larvae (spargana) of genus Spirometra species tapeworms, and it occurs worldwidely. Most of human cases have been occurred in Asian countries including China [
1]. The etiologic agent of this disease, sparganum, is mainly infected through the raw meat consumption of intermediate hosts, frogs and snakes. In human body, it frequently invaded in subcutaneous and/or muscular tissues, and eyes and rarely in central nervous system including brain. In China, the first sparganosis case was reported in Xiamen, Fujian province in 1882. Then 1,359 cases were reported from 1949 to 2014, more than 50 cases in Hunan province [
1]. Most cases are subcutaneous and ocular sparganosis. However, very few cases of spinal sparganosis have been recorded so far. Therefore, we intended to describe a rare human case of lumbosacral canal sparganosis in China.
CASE DESCRIPTION
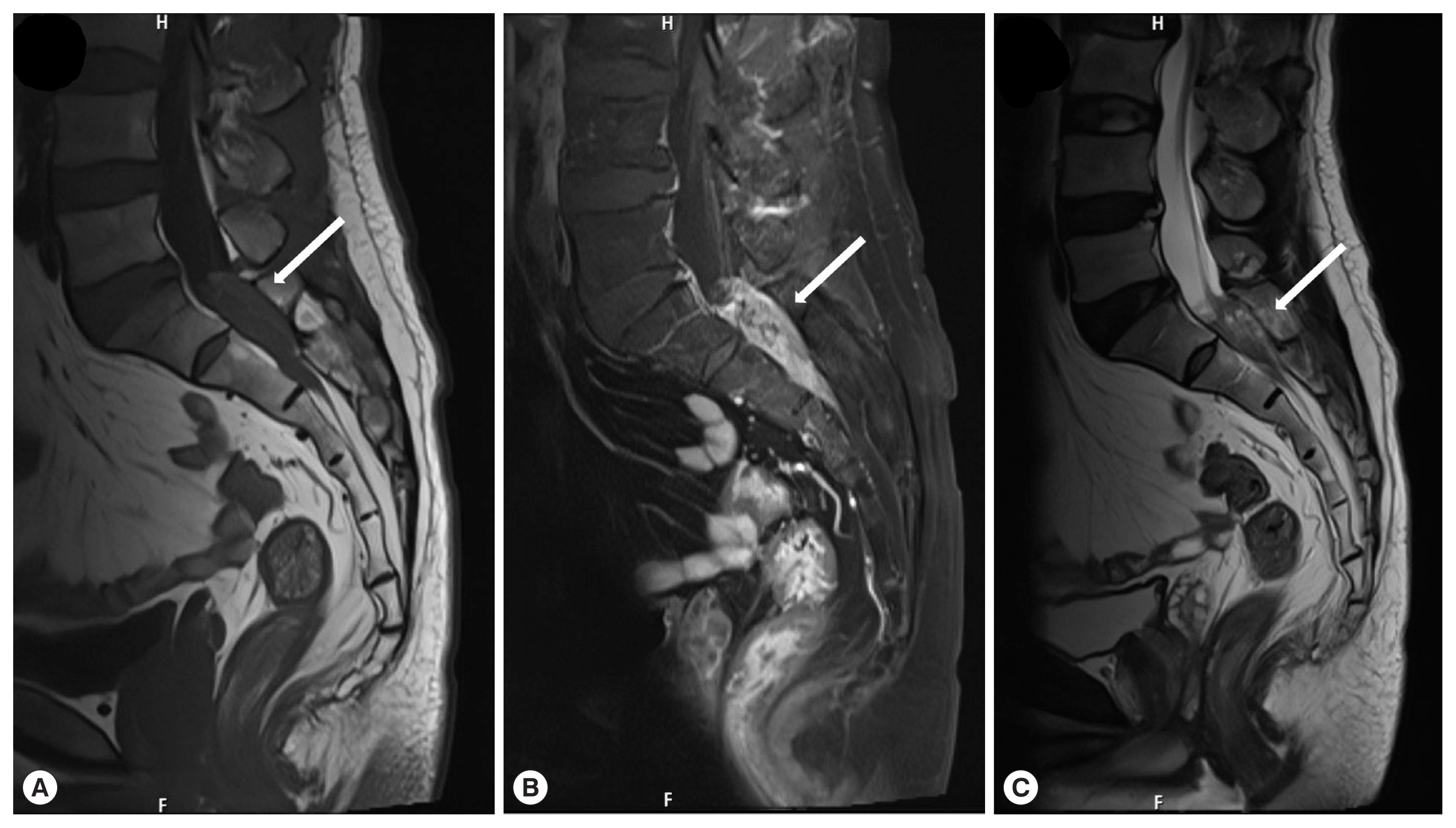
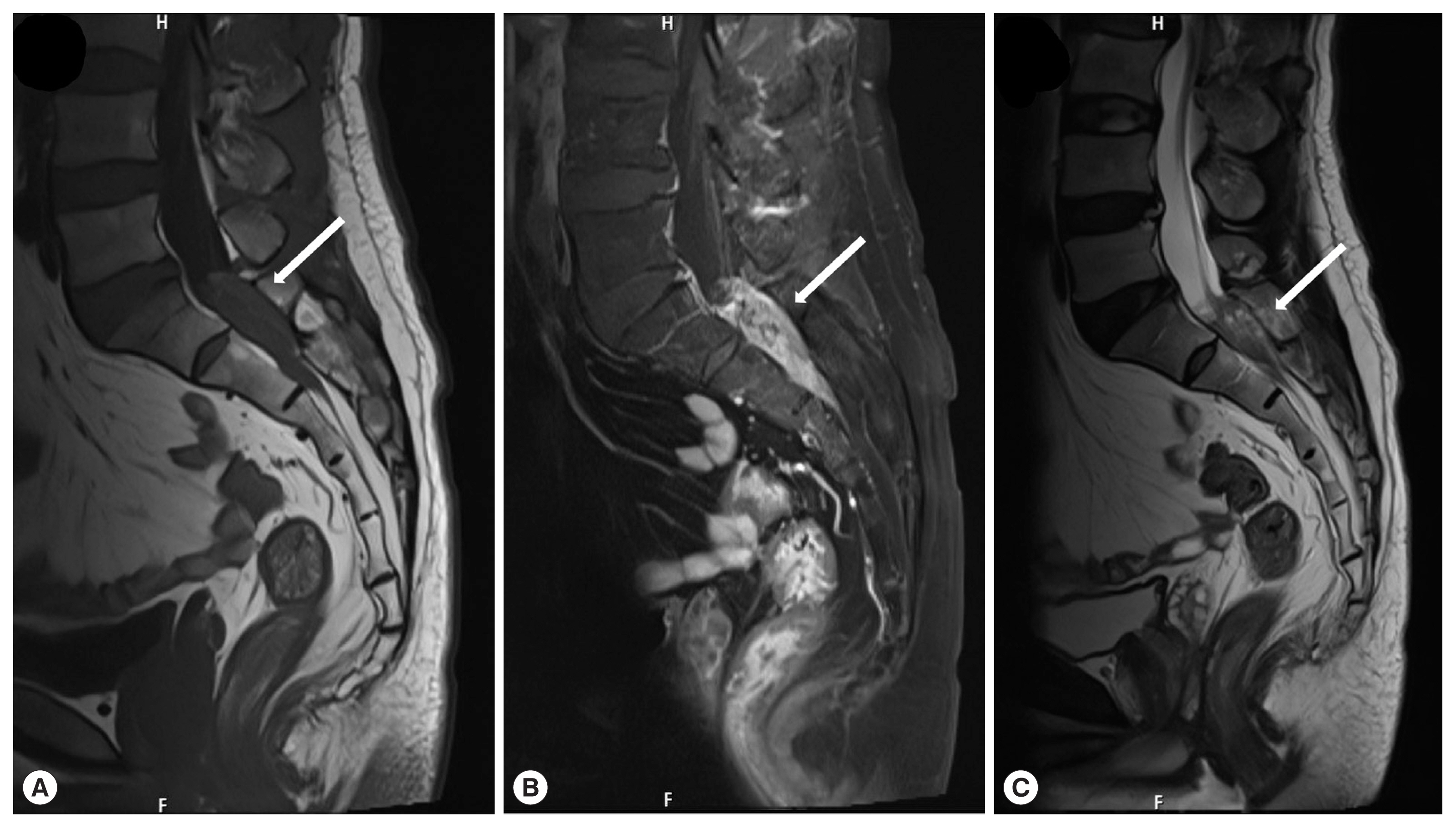
A 56-year-old man presented with a 1-week history of perianal pain. No history of dysuria or difficulties in defecation were reported. And the muscle strength of the bi-upper and bi-lower limbs was grade 5 in the MRC scale. The muscle tonus of the 4 limbs was normal, with normal tendon reflexes in the upper and lower limbs. And laboratory assessment revealed that white blood cell count of 6,200/μl (reference range 4,000–10,000/μl ), with 1.9% eosinophil count (reference range 0.4–8.0%). Further examinations such as blood biochemistry, routine stool examination, and urine analysis were within normal range. MRI of the lumbosacral spine with gadolinium contrast study showed a 1.7×1.5×5.4 cm heterogeneous enhancing mass at the S1–2 level (
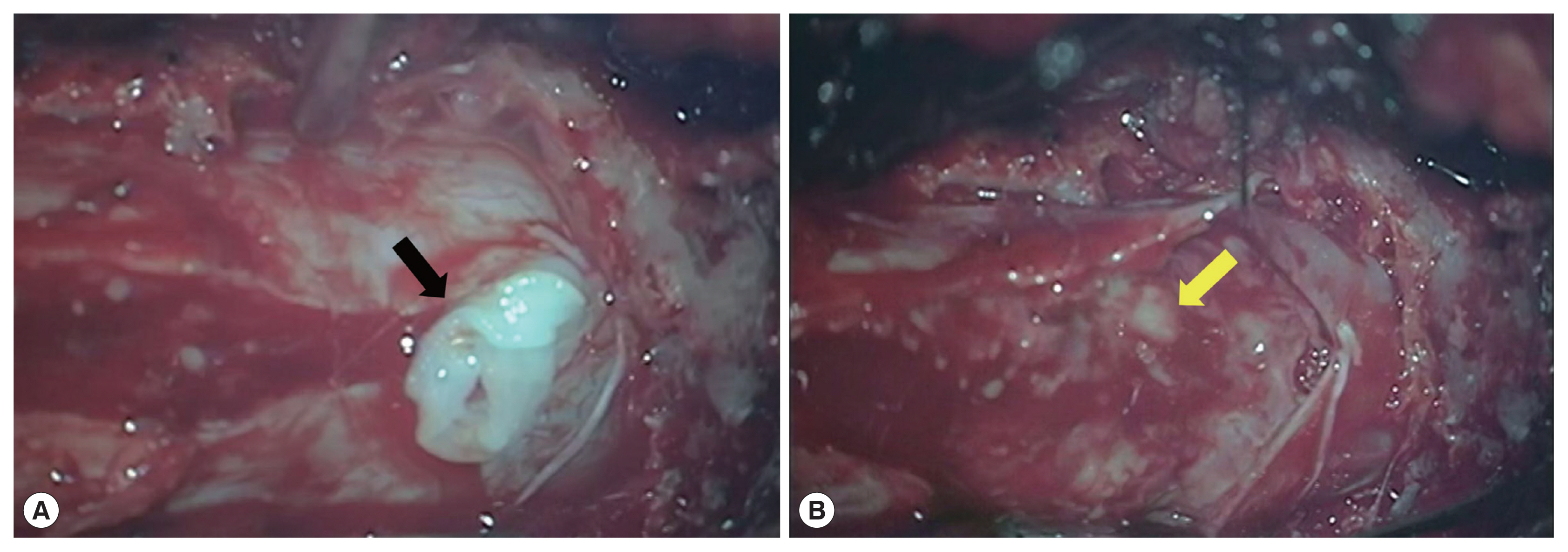
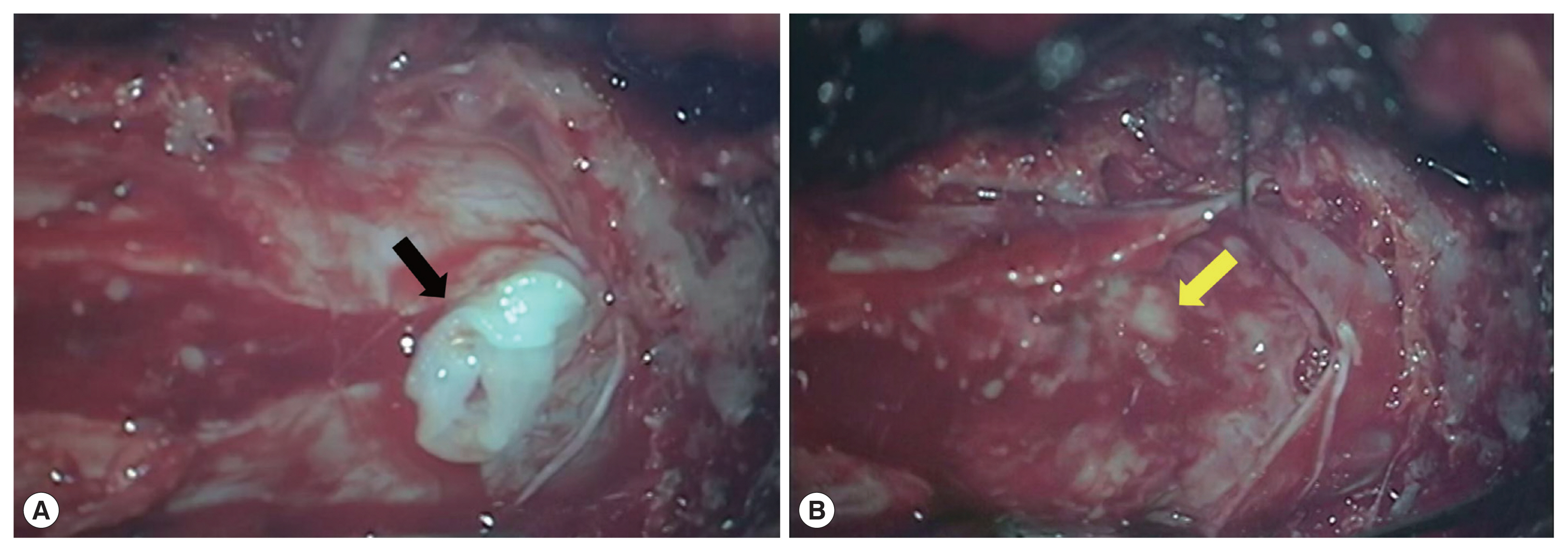
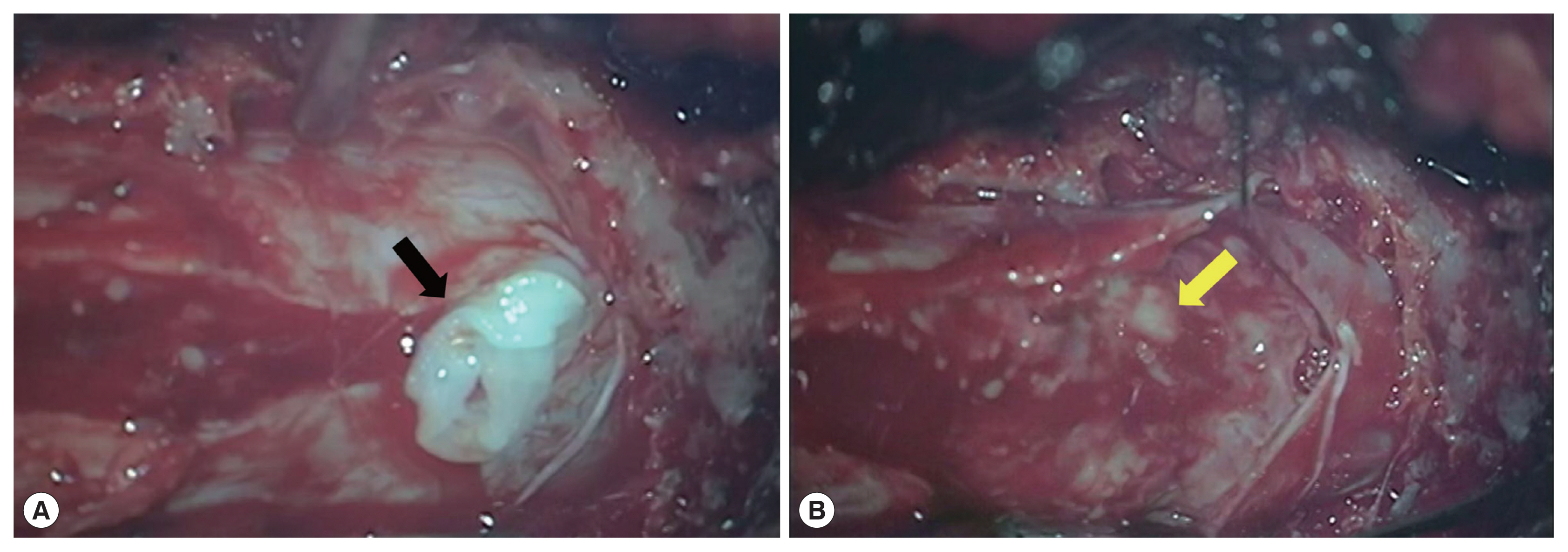
Fig. 1). We initially considered the possibility of a neoplastic lesion. The patient underwent laminectomy from S1 to S2. On the operative view, we found that the dural tension was very high, the arachnoid membrane was thickened and yellowish-white due to severe inflammation and adhesion. We detected a live worm in inferior margin of L5 (
Fig. 2A), proliferative inflammatory granulation tissue (
Fig. 2B) surrounding the nerve tissue of cauda equina, which is not easy to remove. We did not remove inflammatory granulation tissue, just only took the worm body out from it.
On further carefully inquiring, our patient had a history of ingesting undercooked frog meat in his youth. Blood and cerebrospinal fluid samples were further collected and sent to the Department of Parasitology, Xiangya Medical College, Central South University for immunological diagnosis. The specific anti-body IgG against tissue-dwelling parasites (Clonorchis sinensis, Paragonimus westermani, Schistosoma japonicum, Echinococcus granulosus, and Trichinella spiralis) were assayed by ELISA and the results were all negative. But both in CSF and serum sample, the specific anti-sparganum antibody IgG was positive. A dose of praziquantel (50 mg/kg once a day), albendazole (15 mg/kg once a day), and dexamethasone (0.1 mg/kg once a day) was administered to the patient. After 1 month of treatment, the patient’s perianal pain was relieved significantly, but he also had positive anti-sparganum antibody.
DISCUSSION
Sparganosis, a zoonotic parasitic disease caused by the larvae of tapeworms named sparganum, has been recognized worldwide, but it is commonly seen in China, Korea, Japan and eastern Asia. The adult tapeworm parasitizes in small intestine of definitive hosts such as cats, dogs and other carnivores, and their eggs passed to outsides with feces. Under appropriate conditions, the eggs are hatched in water and release coracidia after 2–5weeks. If coracidia are ingested by cyclops, the first intermediate host, then they will develop into procercoid, and when procercoid are swallowed by second intermediate hosts such as amphibians, reptiles and other mammals, especially frogs in which they will accordingly develop into plerocercoid called sparganum [
1]. The majority of sparganum in the human body remain their larval states, but they will invade various tissues and organs of the human body, and cause varying degrees of lesions. They can lodge in human body in the number of dozens, surviving in human tissues for 12 years, or even up to 36 years. There are 3 ways of human infection with sparganum [
2]: (1) Using raw meat or skin from frogs or snakes as poultices; (2) Eating raw or undercooked frog or snake meat and ingestion of live tadpoles; (3) Drinking water contaminated with intermediate hosts. Sparganum can invade the human body through wounds or normal skin and mucous membranes, and then migrate to various tissues of the body. However, the adult
Spirometra mansoni seldom parasitizes the human body and has little pathogenicity to humans [
3]. But the infected patients may be reported with some mild symptoms such as discomfort or slight pain in the epigastrium and central abdomen, even nausea and vomiting. Human sparganosis caused by sparganum is far more harmful than that caused by adult
Spirometra mansoni. Besides, lesions vary with the migration and residence of sparganum. Sparganum could lodge in human eyes, subcutaneous body of limbs, oral and maxillofacial regions, followed by central nervous system lesions. It is also reported that they are found in internal organs such as lungs, scrotal and bladder [
4,
5]. However, lumbosacral spinal canal involvement is extremely rare. Spinal sparganosis patients may present with radicular pain, neurogenic bladder, and paraparesis. In our case, however, the patient showed only perianal pain.
In the case of cerebral sparganosis, the typical signs on Computed tomography (CT) include hypodensity of the white matter, irregular or nodular-enhancing lesions and small dot-like calcification. MRI findings may include aggregated ring-like enhancement (often 3 to 6 bead-shaped rings), “tunnel sign” with enhancement of lesions, and migration of radiographic lesions as larvae migrate. In our case, the lumbosacral MRI revealed heterogeneous enhancing lesion at the S1–2 level. The gold standard for diagnosis of sparganosis remains histological examination [
6]. In addition, IgG antibodies to sparganum from serum or CSF can be detected by ELISA, which has high sensitivity and specificity [
7]. However, the diagnosis mainly depends on surgical detection of the worms due to the rare presence of sparganosis. In our case, the ELISA for anti-sparganum antibodies was positive in both plasma and CSF collected on the day after operation.
In terms of treatment, it is essential to completely remove sparganum even their cephalic segment. The mainly methods are surgical removal of the larva and administration of high-dose praziquantel. Surgically, sparganum should be removed completely and thoroughly in case that the residual scolex leads to recurrence. And as for drug treatment, praziquantel has been proved a suitable option. A recent retrospective study indicated that 94 percent of patients with central nervous system sparganosis have improved radiographically after treating with a high-dose regimen of praziquantel [
8]. As for our patient, the proliferative inflammatory granulation adhered to his nerve tissue of cauda tightly. Therefore, we just took out the live worm rather than removing inflammatory granulation tissue in case of any risks. After operation, the patient has been continuously treated with medicine including praziquantel, albendazole, and dexamethasone. Serological tests were repeated at appropriate intervals to evaluate the efficacy of treatment.
In this study, we diagnosed a case of intraspinal sparganosis with perianal pain. Although MRI showed certain characteristics, its diagnosis mainly depended on the detection of worms during operation and antigen-specific IgG antibodies from peripheral blood or cerebrospinal fluid by ELISA. Although surgical removal of entire worm body is the most effective method for the treatment of sparganosis. However, for lumbosacral canal sparganosis, it adheres closely to the nerve tissue, so it can only be removed as much as possible, and antiparasitic drugs can be added after operation. At present, the symptoms of the patient are relieved, but the long-term prognosis is still unknown. Although spinal sparganosis is a very rare infection disease, the patients who had the history of eating raw or undercook frogs or snakes and drinking contaminated water should be suspected of infecting sparganosis, especially in endemic areas. Preoperative ELISA is useful for the diagnosis so as to figure out a more favorable treatment plan.
Notes
-
All authors declare no conflict of interests.
ACKNOWLEDGMENTS
We would like to acknowledge all staff of the department of neurosurgery at Xiangya Hospital Central South University. This work was supported by the Science and Technology Program of Hunan Province (project number 2021ZK4154) and Graduate Case base construction project of Central South University (project number 2020ALK91).
Fig. 1Magnetic resonance imaging lumbosacral spines, sagittal plane. T1WI (A), gadolinium-enhanced T1WI (B), and T2WI (C) showed a 1.7×1.5×5.4 cm lesion (arrow) at the S1–S2 level. The lesion exhibited mixed isosignal intensity at T1WI, iso/hypersignal intensity at T2WI and heterogeneous and irregular enhancement at T1WI with GD. And there are cystic changes within the lesion.
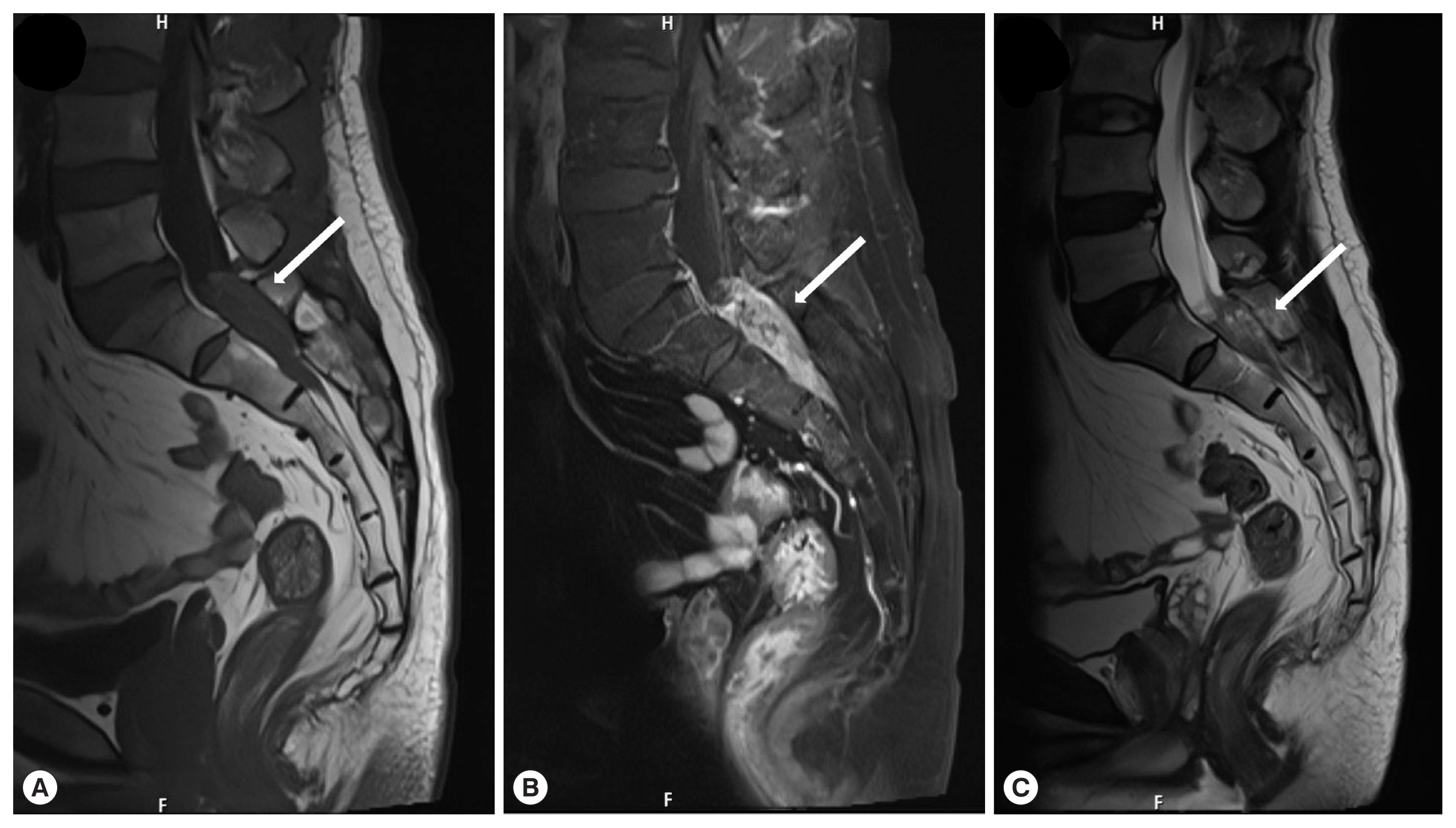
Fig. 2Operative field pictures. (A) After incision of the dura, the live worm (black arrow) was located at inferior margin of L5. (B) After removal of the worm, obvious proliferation of subdural granulation tissue was observed (yellow arrow).
References
- 1. Liu Q, Li MW, Wang ZD, Zhao GH, Zhu XQ. Human sparganosis, a neglected food borne zoonosis. Lancet Infect Dis 2015;15:1226-1235. https://doi.org/10.1016/S1473-3099(15)00133-4
- 2. Lu G, Shi DZ, Lu YJ, Wu LX, Li LH, Rao LY, Yin FF. Retrospective epidemiological analysis of sparganosis in mainland China from 1959 to 2012. Epidemiol Infect 2014;142:2654-2661. https://doi.org/10.1017/S0950268814000144
- 3. Lin XM, Liu CJ, Zhang HW, Zheng LY, Yan QY, He LJ, Zhao XD. Epidemiological investigation on sparganosis mansoni and animal experiments. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 2010;28:132-134. (in Chinese).
- 4. Yun SJ, Park MS, Jeon HK, Kim YJ, Kim WJ, Lee SC. A case of vesical and scrotal sparganosis presenting as a scrotal mass. Korean J Parasitol 2010;48:57-59. https://doi.org/10.3347/kjp.2010.48.1.57
- 5. Matsuki M, Higashiyama A. Pulmonary sparganosis: tunnel sign and migrating sign on computed tomography. Intern Med 2021;60:601-604. https://doi.org/10.2169/internalmedicine.5304-20
- 6. Liao H, Li D, Zhou B, Liu J, Li Y, Liu H, Wu Y, Zhu X, Tan C. Imaging characteristics of cerebral sparganosis with live worms. J Neuroradiol 2016;43:378-383. https://doi.org/10.1016/j.neurad.2016.08.001
- 7. Cui J, Li N, Wang ZQ, Jiang P, Lin XM. Serodiagnosis of experimental sparganum infections of mice and human sparganosis by ELISA using ES antigens of Spirometra mansoni spargana. Parasitol Res 2011;108:1551-1556. https://doi.org/10.1007/s00436-010-2206-2
- 8. Hong D, Xie H, Wan H, An N, Xu C, Zhang J. Efficacy comparison between long-term high-dose praziquantel and surgical therapy for cerebral sparganosis: a multicenter retrospective cohort study. PLoS Negl Trop Dis 2018;12:e0006918. https://doi.org/10.1371/journal.pntd.0006918
Citations
Citations to this article as recorded by

- Infectious Myelopathies
Anita M. Fletcher, Shamik Bhattacharyya
Continuum.2024; 30(1): 133. CrossRef - The serum IgG antibody level as a biomarker for clinical outcome in patients with cerebral sparganosis after treatment
Haijie Xiang, Jie Wang, Dandan Tan, Ying Xiong, Pengcheng Huang, Yu Shen, Yun Xu, Zhihong Gong, Fei Hu, Chunhua Xu, Jie Wu, Wei Liu, Junpu Liu, Hui Wan, Daojun Hong, Huiqun Xie
Frontiers in Immunology.2023;[Epub] CrossRef - Multiple sparganosis spinal infections mainly in the thoracic region: A case report
Gan-Jun Wen, Jian Chen, Shi-Fei Zhang, Zhi-Sen Zhou, Gen-Long Jiao
World Journal of Clinical Cases.2023; 11(36): 8507. CrossRef
 , Sheng Huang1,†
, Sheng Huang1,† , Jing Li2, Ren-Jun Peng1, He Huang1, Xi-Ping Ding1, Li-Ping Jiang2,3,*
, Jing Li2, Ren-Jun Peng1, He Huang1, Xi-Ping Ding1, Li-Ping Jiang2,3,* , Jian Xi1,*
, Jian Xi1,*