Abstract
Toxoplasma gondii is a neurotropic apicomplexan protozoan estimated to affect approximately 30% of the global population. In this review, we aimed to examine scientific evidence on the potential role of T. gondii infection in the development of autism spectrum disorder (ASD), a heterogeneous neurodevelopmental disorder. This review summarizes the current literature exploring the possible association between T. gondii and ASD. Findings indicate that toxoplasmosis may contribute to host alterations, including the induction of humoral and cellular immune responses, production of various cytokines, and changes in neurotransmitter levels (e.g., serotonin, dopamine, acetylcholine, gamma-aminobutyric acid, and glutamate), as well as the activation of enzymes such as indoleamine 2,3-dioxygenase, which may influence the pathophysiology of ASD. In conclusion, this review suggests that T. gondii infection could act as a potential risk factor for ASD. However, further intensive studies are necessary to clarify the role of this parasite in the etiology and progression of ASD. This review is anticipated to stimulate further studies aimed at understanding and potentially reducing the burden of neurodevelopmental disorders worldwide.
-
Key words: Toxoplasma gondii, toxoplasmosis, autism, autism spectrum disorder, neurotransmitter, immune response
Introduction
Autism spectrum disorder (ASD) is a heterogeneous neurodevelopmental disorder characterized by impairments in social interaction and communication as well as by the presence of unusual repetitive behaviors that typically emerge in early childhood [
1,
2]. According to the Autism and Developmental Disabilities Monitoring Network of the US Centers for Disease Control and Prevention, the estimated prevalence of ASD among 8-year-old children in 2020 was 1 in 36—approximately 4% in boys and 1% in girls [
3]. ASD has a multifactorial etiology involving neurological, environmental, immunological, and genetic factors, although the precise role of each factor remains unclear [
4]. These uncertainties have limited the development of effective treatments. Therefore, improving our understanding of the underlying pathology of ASD is essential for identifying new therapeutic approaches for this lifelong condition [
2].
Toxoplasma gondii is an obligate intracellular parasite estimated to infect approximately 25%–30% of individuals in both developed and developing countries [
5–
7]. It invades various host cell types and forms cysts that usually remain dormant throughout the host’s lifetime [
8]. These cysts mostly develop in the brain cells—particularly neurons, astrocytes, and microglia [
9]—as well as in the retina and muscle tissues [
10]. Emerging evidence suggests that latent toxoplasmosis is not only asymptomatic but can also be harmful [
11]. Cysts of
T. gondii have been shown to alter neuronal biological functions, including gene expression and neurotransmitter synthesis, potentially disrupting brain connectivity and contributing to behavioral and neurological impairments [
12–
18]. Recent studies have identified toxoplasmosis as a potential risk factor for several neurodegenerative and neuropsychiatric disorders, including Parkinson disease, Alzheimer disease, schizophrenia, ASD, bipolar disorder, obsessive-compulsive disorder, depression, and suicidality [
8,
12,
19–
27]. However, the pathogenic mechanisms underlying these associations remain unclear. Therefore, this review was designed to examine the potential association between toxoplasmosis and ASD. The risk factors through which
T. gondii infection may influence this relationship are outlined below, and
Table 1 summarizes the key literature supporting these associations [
28–
39].
Immunological Factors
The development of neuropsychiatric disorders associated with
T. gondii is likely mediated by both the host’s immune response to the parasite and the parasite’s biochemical activity. During
T. gondii infection, components of the innate immune system trigger an adaptive immune response by processing antigens and producing cytokines. Microglia, resident macrophages of the central nervous system (CNS), are believed to be the primary cells responsible for limiting the proliferation of
T. gondii in the brain, largely through mechanisms mediated by interferon-gamma (IFN-γ). IFN-γ is a critical cytokine involved in controlling both the acute and chronic stages of toxoplasmosis. Elevated levels of IFN-γ, interleukin (IL)-1, and tumor necrosis factor-alpha (TNF-α) have been observed in the brain following
T. gondii infection. Moreover, administration of anti-IFN-γ antibodies has been shown to increase the severity of toxoplasmic encephalitis [
40]. IFN-γ also stimulates microglia to secrete TNF-α, thus contributing to a regulatory feedback loop in microglial activation. This IFN-γ-mediated microglia activation, along with TNF-α autocrine signaling, likely plays a key role in the defense mechanism of the brain against
T. gondii. Activated microglia can exert direct lethal effects on
T. gondii by secreting IL-1, TNF-α, and inducible nitric oxide synthase or indirectly by interacting with CD4
+ and CD8
+ T cells to produce additional cytokines, such as IL-10, IL-12, and IL-15 [
40].
Immune dysfunction is considered a potential contributing factor to the development of ASD. Several studies have reported the dysfunction of T cells, the presence of autoantibodies in peripheral blood, and elevated levels of proinflammatory cytokines, chemokines, and differentiation factors in patients with ASD [
8,
41].
The populations of CD4
+ and CD8
+ lymphocytes are reduced in children with ASD. An imbalance in T helper 1 and T helper 2 cytokines has also been reported, with a shift favoring the T helper 2 response [
25]. In children with ASD, serum immunoglobulin levels are altered due to a significant increase in total protein and serum concentrations of IgG, IgG2, and IgG4, which may be associated with greater susceptibility to infections [
42]. These alterations in immunoglobulin classes and subclasses represent one mechanism through which the immune system may contribute to the pathogenesis of ASD [
43]. Given that immunoglobulin levels are naturally low at birth and it takes years to reach adult levels—particularly for some isotypes—they are especially relevant in pediatric disorders [
44]. Several studies examining immunoglobulin profiles in patients with ASD have found decreased serum IgA [
45], elevated plasma concentrations of IgM and IgG [
42,
46], and increased total IgE [
47]. If such abnormal immune activity occurs during vulnerable and sensitive periods of neurodevelopment, it may result in neurological impairments characteristic of ASD. Elevated serum IgG levels in individuals with ASD may contribute to underlying autoimmune processes and/or increased infection risk. The binding of IgG to epithelial cell surfaces, infiltration of lymphocytes, and increased cellular proliferation in the small intestines of children with ASD suggest a higher likelihood of autoimmunity in severe cases [
46]. A systematic review and meta-analysis reported an overall odds ratio of 1.93 for anti-
T. gondii IgG antibodies in patients with ASD compared to controls, indicating a potential association between
T. gondii infection and ASD pathogenesis. However, no significant difference was observed in the anti-
T. gondii IgM antibody levels between patients with ASD and controls [
48]. During
T. gondii infection, IgG antibodies typically appear approximately 2 weeks after the onset of IgM, peak within 2–3 months, and then gradually decline to lower levels, remaining detectable for life due to the persistence of cysts in immune-privileged organs [
49,
50]. Conversely, IgM antibodies serve as indicators of recent infection, appearing about 1-week postinfection, peaking after approximately 1 month, and declining to undetectable levels over the following months [
51].
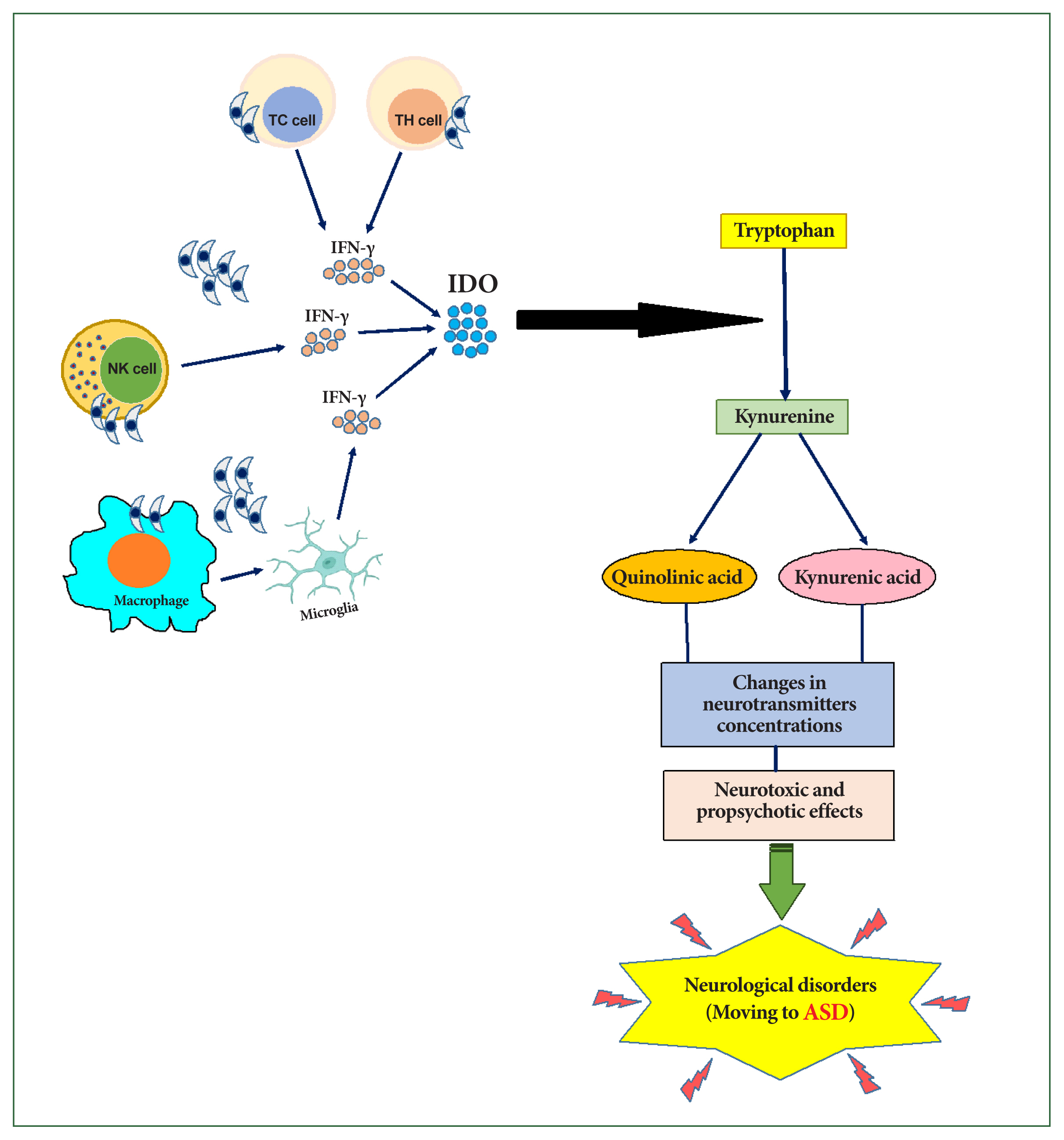
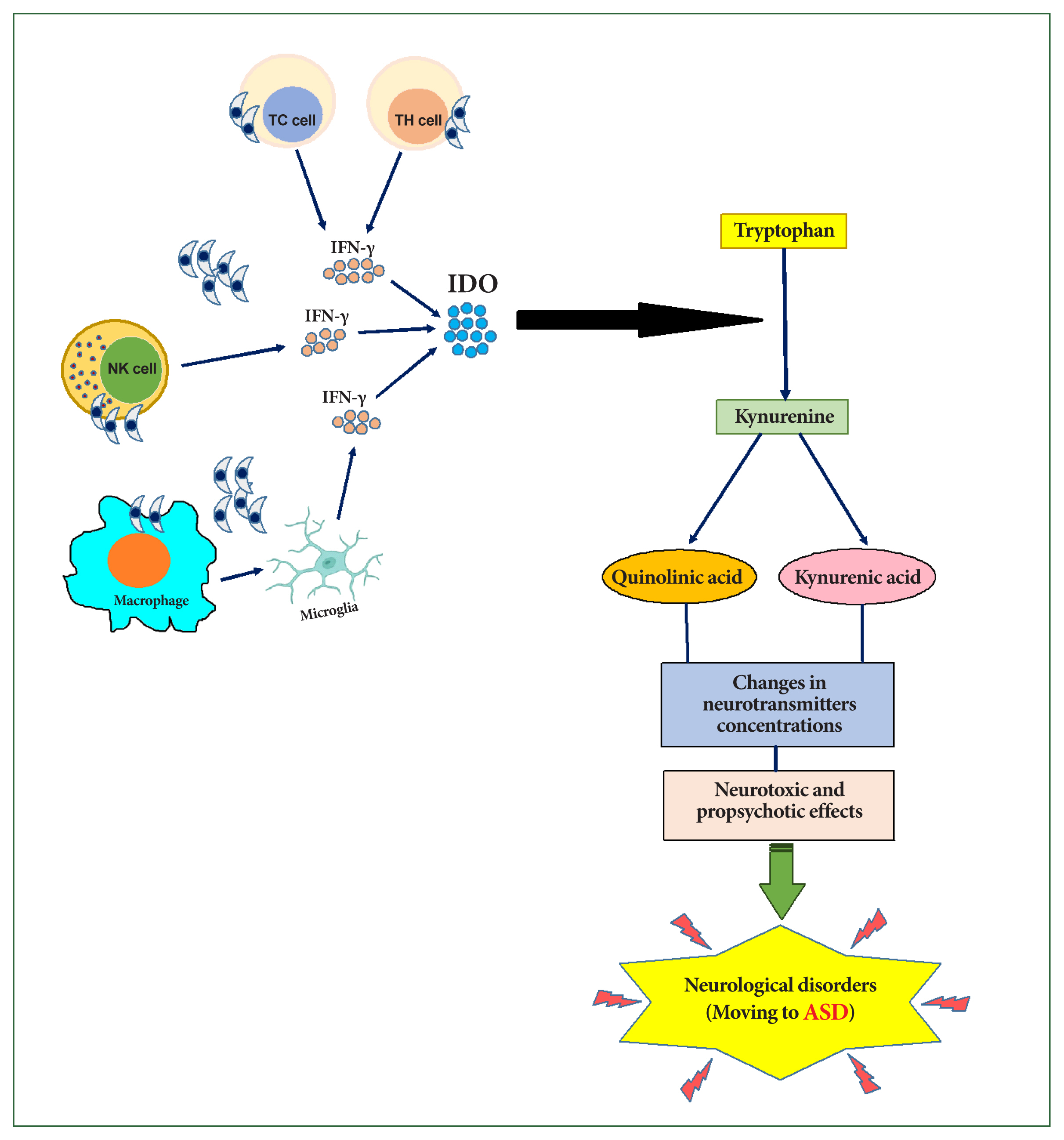
Kynurenine Metabolic Pathway
During
T. gondii infection, IFN-γ and other cytokines produced by neurons, glial cells, natural killer cells, and T lymphocytes play an essential role in the formation of neurodegeneration and oxidative stress associated with ASD [
25]. Oxidative stress results from a biological imbalance between reactive oxygen species and antioxidants, leading to changes in biomolecules and the disruption of intracellular redox-related signaling pathways [
52]. Natural killer cells are activated early in toxoplasmosis by IL-12 and produce high levels of IFN-γ, which helps control the parasite before T-cell activation [
53]. IFN-γ inhibits
T. gondii growth by inducing the release of indoleamine 2,3-dioxygenase (IDO), which in turn catalyzes the degradation of tryptophan [
28]. The depletion of tryptophan inhibits the growth of the tachyzoite form of
T. gondii [
29].
Tryptophan is degraded by the IDO enzyme into kynurenine, which is further hydroxylated into quinolinic acid, a potent N-methyl-D-aspartate receptor, or metabolized into kynurenic acid, an endogenous antagonist of the glutamate N-methyl-D-aspartate receptor [
54]. These metabolites exert neurotoxic effects (quinolinic acid) and propsychotic effects (kynurenic acid), potentially disrupting the neurotransmitter balance (
Fig. 1) [
55].
Stimulation of the kynurenine metabolic pathway following
T. gondii infection may represent a host defense mechanism against pathogen infections [
56]. However, high levels of kynurenic acid and quinolinic acid have been linked to various neurological disorders. Schwartz [
57] suggested that abnormal tryptophan metabolism may serve as a unifying biochemical basis for ASD progression.
Significant decreases in tryptophan levels have been observed in the serum and brain of mice infected with
T. gondii [
30–
32]. Correspondingly, studies have reported substantial increases in kynurenine levels in either serum or brain following toxoplasmosis [
31,
32]. Maximal changes in both tryptophan and kynurenine levels were detected between days 5 and 20 postinfection [
32]. Inflammatory processes thus notably shift the tryptophan pathway toward kynurenine metabolites, disrupting the balance between physiological function and neurotoxicity (
Fig. 1).
Given the clinical features of congenital toxoplasmosis, such as intracranial calcifications, hydrocephalus, and intellectual dysfunction [
58],
T. gondii may be considered a risk factor for ASD. Delayed motor development and intellectual dysfunction are common among children exposed to the parasite in utero, with some remaining asymptomatic until school age [
59,
60].
This evidence supports a potential link between neuroinflammation, kynurenine, and ASD. Since kynurenine can affect various neurotransmitter systems and is influenced by environmental factors, including infection, stress, and inflammation, it is plausible that kynurenine plays a central role in ASD etiology [
61].
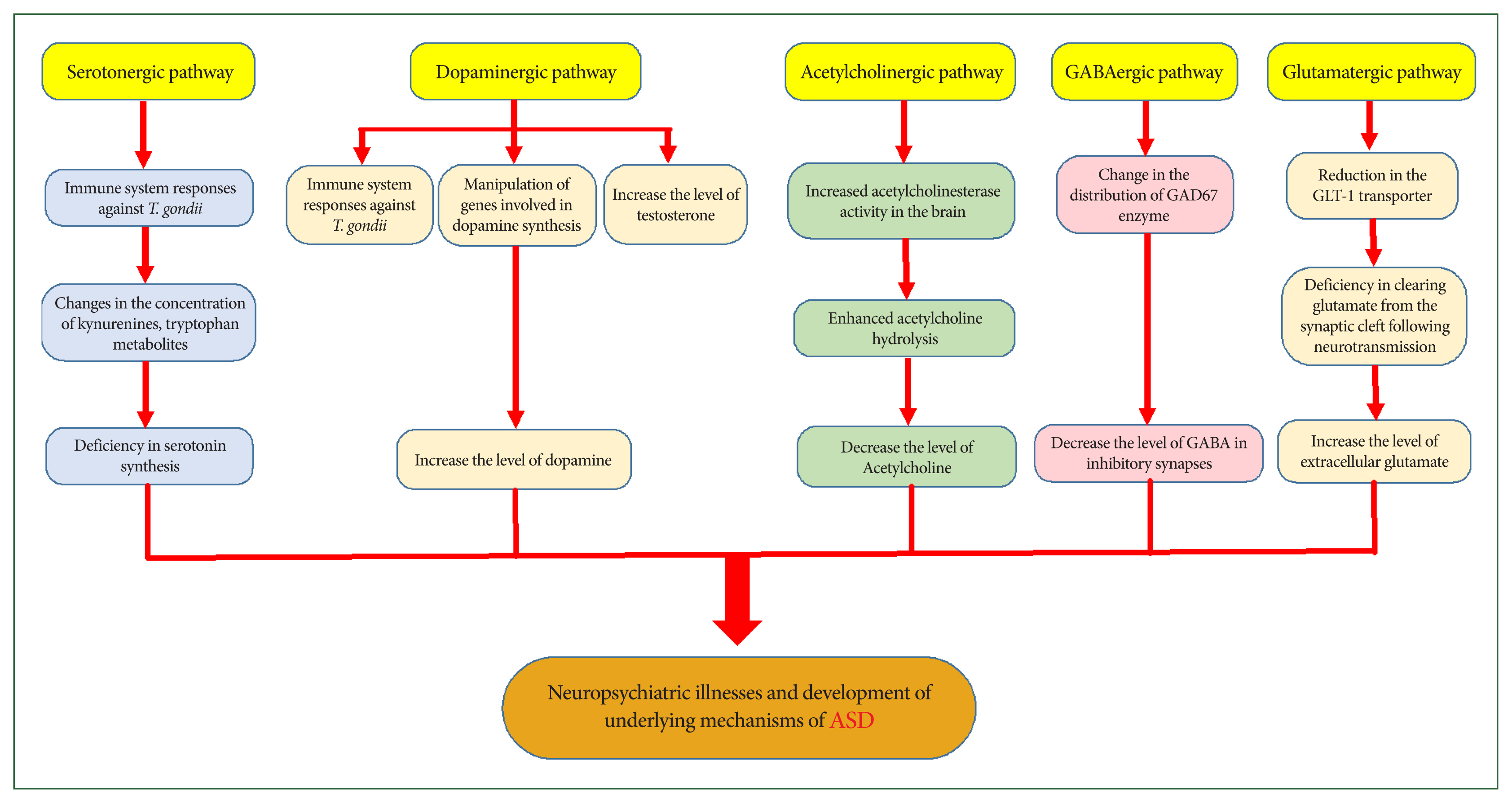
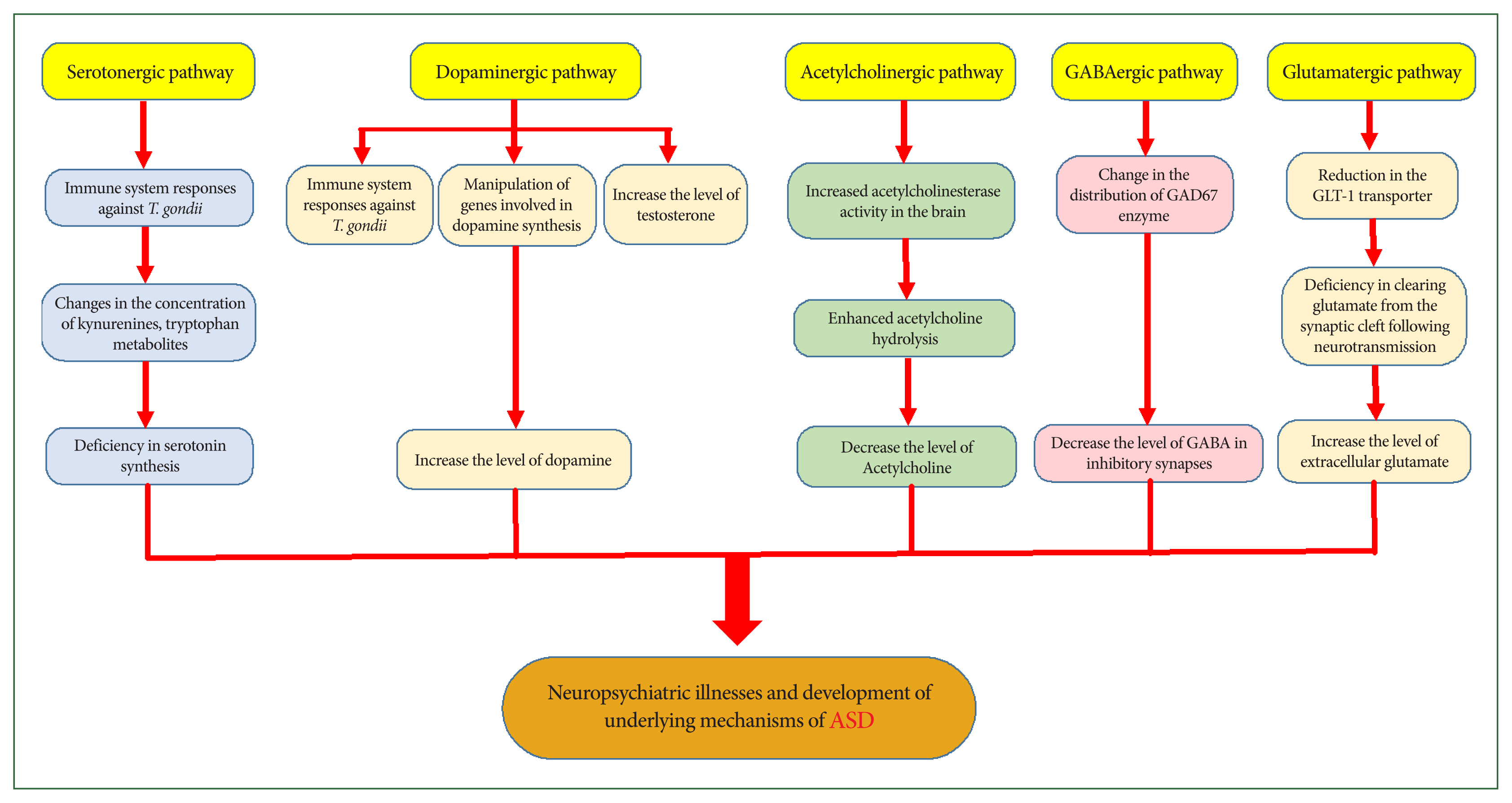
Chronic toxoplasmosis induces specific neuropsychiatric symptoms and behavioral changes in humans and animals; however, the mechanisms responsible for these changes are not fully understood. Parasite-induced alterations in CNS neurotransmitters are among the most essential factors implicated in these psychiatric consequences (
Fig. 2) [
11,
33–
35].
The response of the immune system to
T. gondii may alter neurotransmitter concentrations by modifying the concentrations of kynurenines, tryptophan metabolites, and other endogenous brain compounds [
62]. Serotonin (5-HT) plays an important neurotrophic role during brain development, and abnormalities in CNS concentration can disrupt its functions. Tryptophan is an essential substrate for serotonin synthesis [
63]. Serotonergic abnormalities, along with related cortical development disruptions, are common mechanistic features of ASD. An initial deficiency in serotonin synthesis may affect extensive brain regions, contributing to mood alterations, impaired social interaction, sleep disturbances, aggression, and obsessive-compulsive behaviors reported in ASD [
64–
66]. Research suggests that serotonin-related psychiatric disorders, such as hyperserotonemia, occur in 25%–50% of individuals with ASD and their first-degree relatives, particularly their parents [
67,
68].
Furthermore,
T. gondii directly and indirectly affects dopaminergic signaling and activates the kynurenine metabolic pathway, diverting tryptophan away from serotonin production [
69]. Host immune responses to
T. gondii infection induce T helper 1 differentiation and the production of IFN-γ cytokine, which stimulates IDO enzyme activity to inhibit parasite growth. Activation of this enzyme depletes tryptophan reserves, thereby reducing serotonin synthesis in the brain [
36]. This reduction may contribute to neuropsychiatric disorders and is particularly critical in cases of congenital toxoplasmosis, as studies have shown that abnormal serotonin levels during prenatal and early postnatal development, together with cortical developmental alterations, may predispose individuals to ASD (
Fig. 2) [
64].
Dopamine and the Dopaminergic Pathway
Dopamine is a neurotransmitter that plays a central role in reward-motivated behavior and motor control, and its dysfunction has been implicated in various neurological and psychiatric disorders [
70]. Among the numerous genes manipulated by
T. gondii in an infected host is one that encodes the enzyme tyrosine hydroxylase, which is involved in synthesizing the dopamine neurotransmitter—often referred to as the “pleasure molecule” [
35,
71]. Evidence suggests that increased testosterone levels during chronic toxoplasmosis may enhance dopamine production and that
T. gondii can also synthesize dopamine [
37,
72]. Nitric oxide, IL-2, and IL-6, which are produced by the host immune response to the parasite, further stimulate dopamine release [
72]. Consequently, as shown in both human and animal studies, chronic toxoplasmosis leads to elevated dopamine concentrations in the CNS, and dopamine dysfunction has long been associated with various neuropsychiatric disorders (
Fig. 2) [
11,
35,
73,
74]. Notably, individuals with ASD often exhibit high dopamine levels, and antipsychotic medications that block dopamine receptors are among the most effective treatments for ASD, supporting a significant role for dopamine in the manifestation of ASD symptoms [
65,
75].
Acetylcholine
Acetylcholine is a neurotransmitter that may play a key role in the relationship between latent toxoplasmosis and ASD, as alterations in acetylcholine or its receptors have been reported in both conditions and are potentially linked to specific neurological and behavioral symptoms. Acetylcholine affects the brain by binding to nicotinic and muscarinic acetylcholine receptors (nAChR and mAChR, respectively). The concentration of acetylcholine in the synaptic cleft is regulated by acetylcholinesterase, a membrane-bound enzyme that hydrolyzes acetylcholine, thereby terminating its synaptic activity [
34,
76]. According to existing studies,
T. gondii infection is associated with increased acetylcholinesterase activity in the brain, leading to the enhanced hydrolysis of acetylcholine in the synaptic cleft and a corresponding decrease in its levels in the CNS. Given the proposed anti-inflammatory function of acetylcholine, this decrease may contribute to maintaining inflammatory processes and host defense mechanisms against the parasite. Such processes may underlie brain dysfunctions related to toxoplasmosis, including abnormalities in behavior, locomotion, memory, balance, and orientation [
34,
38]. Evidence further suggests that the cholinergic system is involved in ASD pathogenesis, as exhibited by reductions in neuronal nAChR in the brain cortex, defective acetylcholine signal transduction, lower baseline levels of extracellular acetylcholine, and abnormal acetylcholinesterase activity (
Fig. 2) [
76–
78]. Thus, disruptions in the cholinergic system associated with toxoplasmosis may contribute to neuropsychiatric disorders that are also characteristic of ASD.
Gamma-aminobutyric Acid
Gamma-aminobutyric acid (GABA) is the primary inhibitory neurotransmitter in the CNS, regulating the flow and timing of excitatory neurotransmission [
33]. Beyond its role in neurotransmission, GABA is involved in various cellular processes, such as proliferation, differentiation, migration, synapse organization, axonal development, and neuronal death [
79]. Glutamate decarboxylase (GAD), the key enzyme that catalyzes the conversion of glutamate to GABA at inhibitory synapses, exists in two isoforms—GAD65 and GAD67 [
79,
80]. Studies have shown that GAD65 and GAD67 levels are decreased in the brains of individuals with ASD, resulting in reduced GABA levels and enhanced glutamate concentrations [
80,
81]. Notably,
T. gondii disrupts inhibitory GABAergic synaptic transmission [
33,
37], a process implicated in the pathogenesis of neuropsychiatric disorders such as ASD [
80,
81]. One parasite-induced alteration involves changes in the distribution of the GAD67 enzyme in the brains of individuals with toxoplasmosis. This alteration is associated with spontaneous seizures and may indicate GABAergic system deficits and a loss of neuronal inhibition (
Fig. 2) [
33,
37]. Furthermore,
T. gondii utilizes GABA as a carbon source for its metabolism. The intracellular localization of live parasites induces GABA secretion in parasitized dendritic cells (DCs), which facilitates parasite dissemination by stimulating DC motility. Thus, the parasite manipulates GABAergic signaling in DCs to enhance its dissemination and survival [
33,
79].
Glutamate
Glutamate, the primary excitatory neurotransmitter in the CNS, plays a crucial role in neuronal plasticity and cognitive function. However, excessive or unregulated glutamate levels can lead to neuroexcitotoxicity and neuronal cell death, processes implicated in the pathophysiology of several neuropsychiatric disorders, including ASD [
39,
80,
82]. Glutamate is fully synthesized de novo within the CNS by astrocytes and neurons, which also contributes to the immune response against
T. gondii. Astrocytes regulate glutamate levels in the CNS through uptake, release, conversion into glutamine, and synthesis from precursors, such as lactate, alanine, or α-ketoglutarate. Neurons convert glutamine to glutamate through the glutaminase enzyme [
39]. Toxoplasmosis infection results in a substantial reduction in the astrocytic glutamate transporter, which is essential for clearing glutamate from the synaptic cleft following neurotransmission, leading to a significant increase in extracellular glutamate concentrations (
Fig. 2) [
37,
39]. These findings indicate that abnormalities in glutamatergic neurotransmission caused by
T. gondii may contribute to the neurophysiological mechanisms underlying ASD.
Gender
Sex differences have been observed in hosts with toxoplasmosis regarding susceptibility to infection, immune responses, alterations in brain neurotransmitter levels, and parasite-induced behavioral and personality changes [
83–
87]. Experimental studies have revealed that female mice are more susceptible to acute infection than male mice. Among those who survive and progress to chronic infection, females tend to have a higher cyst burden in the brain than their male counterparts [
84,
85]. Further immunological examination revealed differences in innate and adaptive immune responses—such as cytokine production, cell proliferation, and immune cell activity—which may explain the poor survival rates and higher cyst burdens in female mice [
84,
85]. Additional studies have highlighted the role of sex hormones as potential modulators of these sex-specific immune responses [
88–
90]. Notably, changes in neurotransmitter levels—believed to influence intermediate host behavior during
T. gondii infection—also show sex-dependent patterns [
83]. These sex-dependent effects on the essential molecular pathways of the host body suggest that
T. gondii may play differing roles in the progression of ASD between males and females. Meanwhile, epidemiological studies consistently report a lower prevalence of ASD in females than males, possibly due to sex-specific genetic and hormonal influences, although the underlying mechanisms remain unclear [
91–
93]. Therefore, further research is needed to clarify these uncertainties and elucidate how
T. gondii may differentially affect ASD progression across the sexes.
Genetics and Environmental Factors
ASD encompasses a group of distinct disorders that are strongly influenced by genetics and environmental factors, although the precise underlying causes remain unclear [
94,
95]. The heritability of ASD is approximately 61%–94% [
96]. Twin and family studies report concordance rates for ASD diagnosis of approximately 98% in monozygotic twins and 53% in dizygotic twins, with lower concordance observed in nontwin siblings and markedly lower prevalence in the general population [
94].
Environmental factors are also implicated in ASD risk, spanning prenatal, natal, and postnatal periods. These include maternal infection or depression during pregnancy, abnormal interpregnancy intervals (both short and long), increased maternal body mass index, prenatal exposure to radiation and sodium valproate, cesarean delivery, gestational age at birth, low birth weight, and measles, mumps, and rubella vaccination [
94,
95,
97].
Conclusion
This review shows that T. gondii infection constitutes a significant risk factor for ASD. The changes induced by toxoplasmosis in the host—including the activation of humoral and cellular immune responses, the production of various cytokines, changes in neurotransmitter levels (e.g., serotonin, dopamine, acetylcholine, GABA, and glutamate), and the activation of enzymes such as IDO—may contribute to the development and progression of ASD.
Moreover, further intensive studies are necessary to clarify the effects of this parasite on the etiology and progression of ASD. Elucidating the mechanisms involved in host-parasite interactions and examining the role of parasite genotypes in these processes is essential to advancing our understanding of the association between toxoplasmosis and ASD. Given that various
T. gondii strains exhibit varying pathogenicity and elicit distinct immune responses in the host, infections caused by these strains likely have differential impacts on the course of neurodegenerative and neurodevelopmental disorders, as suggested by recent studies [
98,
99]. It is hoped that the findings of this review will guide future studies aimed at reducing the burden of mental disorders globally.
Notes
-
Author contributions
Conceptualization: Khalilian A, Daryani A
Data curation: Mikaeili Galeh T, Nayeri T, Dodangeh S, Hosseininejad Z, Tanzifi A
Investigation: Mikaeili Galeh T, Nayeri T, Dodangeh S, Hosseininejad Z, Tanzifi A
Methodology: Khalilian A
Project administration: Mikaeili Galeh T, Daryani A
Supervision: Daryani A
Validation: Mikaeili Galeh T
Writing – original draft: Mikaeili Galeh T, Nayeri T, Dodangeh S, Hosseininejad Z, Tanzifi A
Writing – review & editing: Mikaeili Galeh T, Daryani A
-
Conflict of interest
The authors declare no conflict of interest related to this study.
-
Acknowledgments
The authors thank Khoy University of Medical Sciences for approving this research (approval No. 402000029) under the ethics code IR.KHOY.REC.1402.051.
Fig. 1Role of interferon-gamma (IFN-γ) in stimulating the kynurenine metabolic pathway following Toxoplasma gondii infection, contributing to neurological disorders. IDO, indoleamine 2,3-dioxygenase; ASD, autism spectrum disorder.
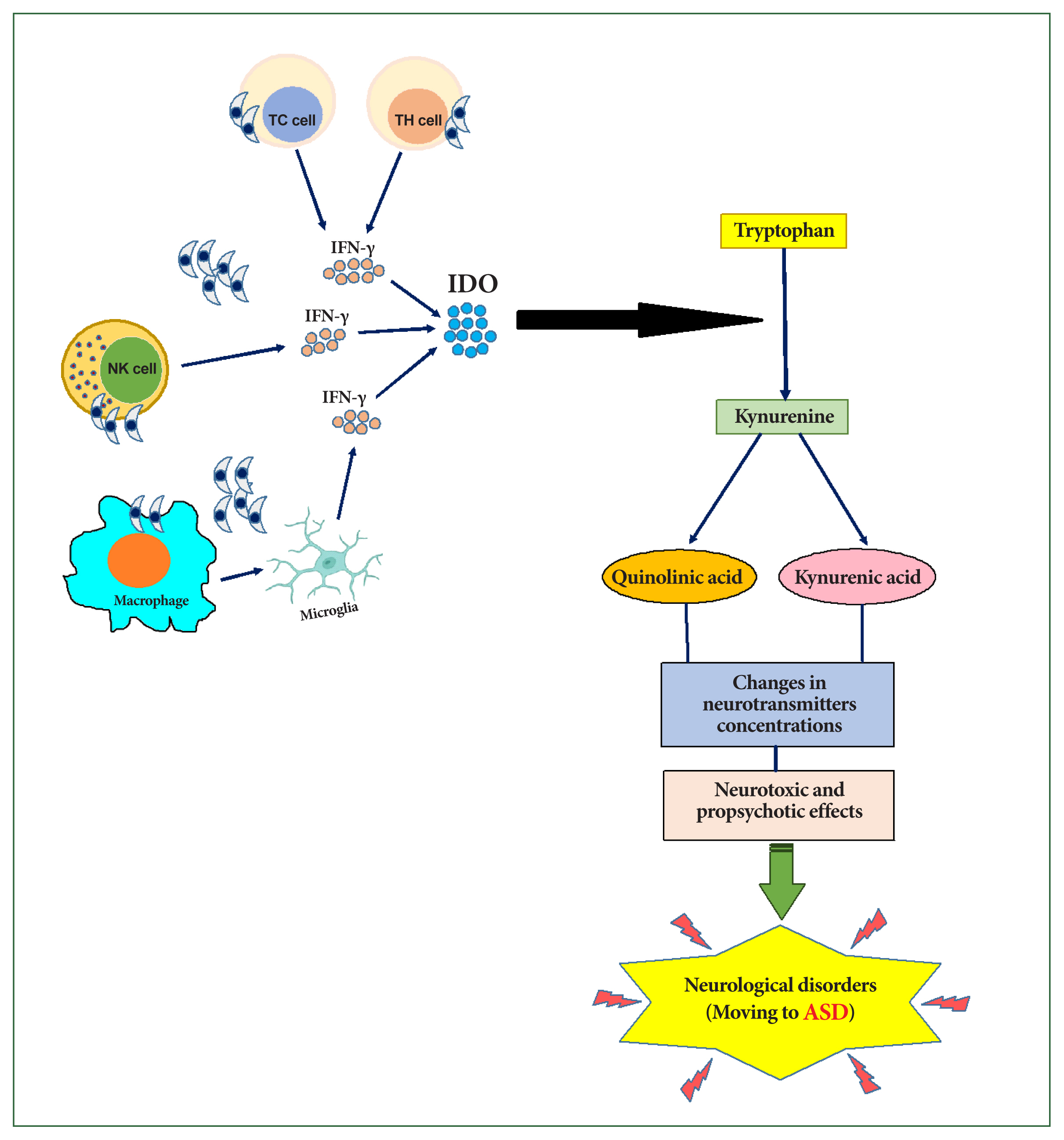
Fig. 2Effects of toxoplasmosis on neurotransmitter pathways in the central nervous system, ultimately leading to neurological disorders. GAD, glutamate decarboxylase; GABA, gamma-aminobutyric acid; GLT-1, glutamate transporter-1; ASD, autism spectrum disorder.
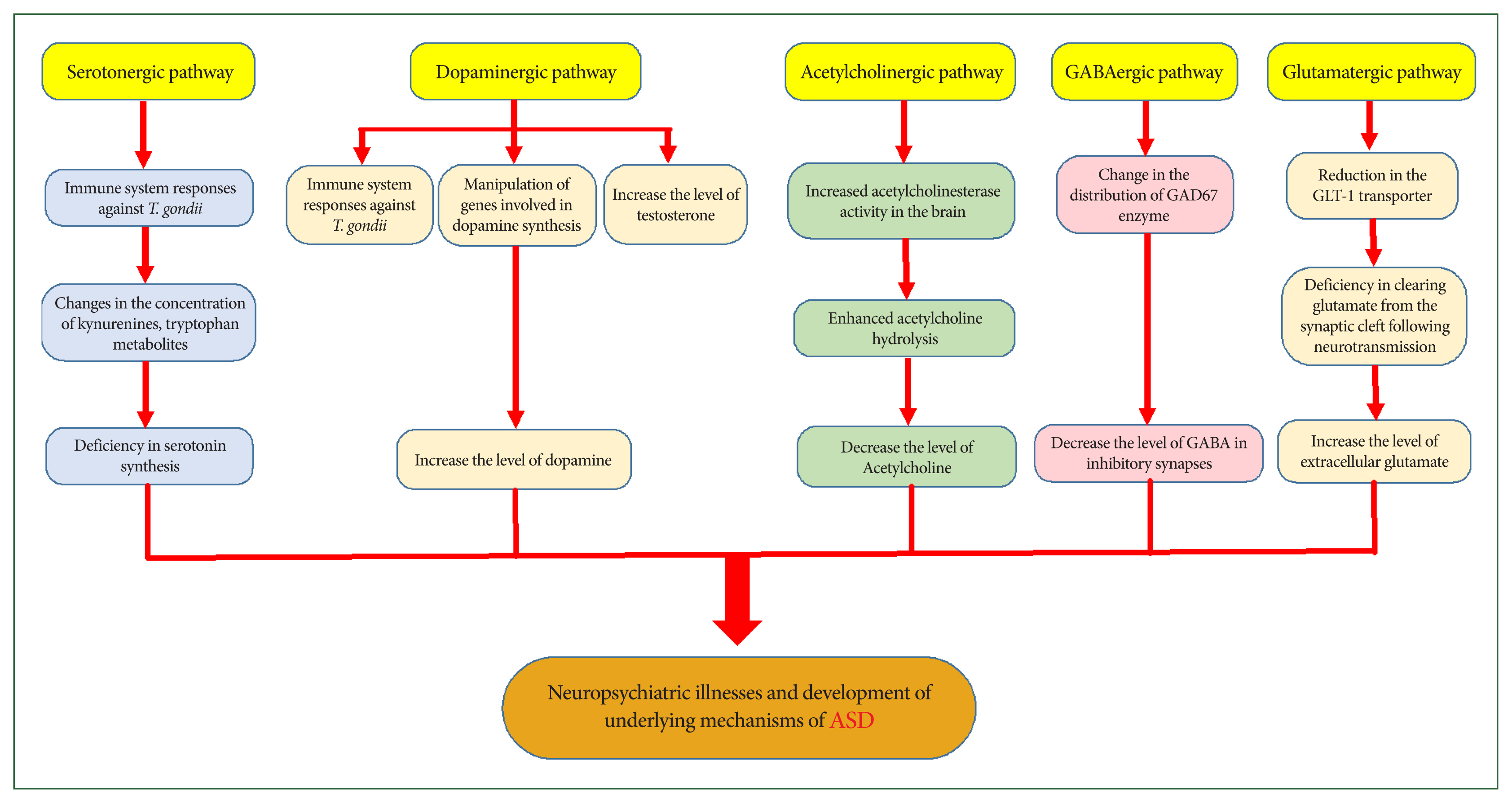
Table 1Key literature supporting the role of Toxoplasma gondii infection as a risk factor for autism spectrum disorder
Table 1
|
Author (year) |
Country |
Study type |
Host/culture media |
T. gondii strain |
Sample |
Diagnostic technique |
Key finding |
|
Pfefferkorn (1984) [28] |
Germany |
In vitro study |
Human fibroblast cultures |
RH |
Human fibroblast cultures |
Chromatography, Electrophoresis, etc. |
INF-γ blocks T. gondii growth in human fibroblasts by inducing host cell degradation of tryptophan |
|
Stibbs (1985) [29] |
USA |
Animal study |
Swiss-Webster mice |
C56 |
Brain |
HPLC |
Increased dopamine levels in T. gondii-infected mice |
|
Fujigaki et al. (2002) [31] |
Japan |
Animal study |
C57BL/6J and IFN-γ-gene-deficient (knockout) mice |
Fukaya |
Lung, Brain, Plasma |
HPLC, RT-PCR |
Significant increase in IDO enzyme activity and mRNA levels in lungs and brain, and a substantial reduction in lung L-tryptophan concentrations following T. gondii infection in C57BL/6J mice
These metabolic changes were absent in T. gondii-infected and uninfected IFN-γ gene-deficient mice |
|
Silva et al. (2002) [32] |
Brazil |
Animal study |
129, C57BL/6, IFN-γ−/− mice |
ME-49 |
Serum, Liver, Spleen, Lungs, Brain |
HPLC, RT-PCR |
Decreased tryptophan and increased kynurenine in the lungs, brain, and serum from mice infected with T. gondii
Absence of induction of IDO mRNA expression, tryptophan degradation, and kynurenine formation in tissues from mice deficient in IFN-γ (IFN-γ−/−) |
|
Engin et al. (2012) [30] |
Turkey |
Animal study |
House mice |
RH |
Serum |
HPLC |
Higher kynurenine/tryptophan ratio in mice infected with T. gondii
|
|
Tonin et al. (2014) [34] |
Brazil |
Animal study |
BALB/c mice |
RH, VEG, ME-49 |
Brain, Serum |
Spectrophotometric method, modified Griess assay |
Increase AChE activity and nitric oxide levels in the brains of mice infected with T. gondii
|
|
Brooks et al. (2015) [33] |
USA |
Animal study |
C57BL/6 mice |
ME-49 and CEP |
Brain |
Immunohistochemistry, Western blot, RT-PCR |
Altered GABAergic synapses and signaling with oss of GAD67 at synaptic terminals; spontaneous seizures in mice infected with T. gondii
|
|
David et al. (2016) [39] |
USA |
Animal study |
C57BL/6 or BALB/c mice |
ME-49 |
Brain |
Real-time PCR, Western blot, Immunohistochemistry, Microdialysis |
A significant reduction in GLT-1 expression, a significant increase in extracellular concentrations of glutamate, and neuronal morphology changes, including dendritic spine loss following infection with T. gondii
|
|
Machado et al. (2016) [38] |
Brazil |
Animal study |
Mice |
ME-49 |
Brain |
Photometric method, Behavioral tests |
Increase brain AChE activity, memory impairment, and anxiolytic behavior in mice infected with T. gondii
|
|
AL-Hadad et al. (2019) [35] |
Iraq |
Human study |
Human |
- |
Serum |
ELISA |
Slight increase in serum dopamine levels in infected individuals |
|
Atmaca (2019) [36] |
Turkey |
Animal study |
Swiss albino mice |
ME-49 |
Brain |
RT-PCR |
Increased expression of serotonin receptors (5-HTR2A, 5-HTR2C, 5-HTR6, 5-HTR7) in mice infected with T. gondii
|
|
Carrillo et al. (2020) [37] |
Iran |
Animal study |
C57BL/6J and Cx3cr1-GFP mice |
ME49, ME49-RFP, and CEP |
Brain |
Immunohistochemistry, Serial block-face scanning electron microscopy |
Loss of inhibitory perisomatic synapse and microglial activation following persistent T. gondii infection |
References
- 1. Esnafoglu E, Demir EY, Cetinkol Y, Calgin MK, Erdil A, et al. The seroprevalence of antibodies to Toxoplasma gondii among children with autism. Dusunen Adam J Psychiatry Neurol Sci 2017;30(4):309-315. https://doi.org/10.5350/DAJPN2017300404
- 2. Gesundheit B, Rosenzweig JP, Naor D, Lerer B, Zachor DA, et al. Immunological and autoimmune considerations of autism spectrum disorders. J Autoimmun 2013;44:1-7. https://doi.org/10.1016/j.jaut.2013.05.005
- 3. Maenner MJ, Warren Z, Williams AR, Amoakohene E, Bakian AV, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2020. MMWR Surveill Summ 2023;72(2):1-14. https://doi.org/10.15585/mmwr.ss7202a1
- 4. Ashwood P, Wills S, Van de Water J. The immune response in autism: a new frontier for autism research. J Leukoc Biol 2006;80(1):1-15. https://doi.org/10.1189/jlb.1205707
- 5. Nayeri Chegeni T, Sharif M, Sarvi S, Moosazadeh M, Montazeri M, et al. Is there any association between Toxoplasma gondii infection and depression? A systematic review and meta-analysis. PLoS One 2019;14(6):e0218524. https://doi.org/10.1371/journal.pone.0218524
- 6. Dubey JP. The history of Toxoplasma gondii: the first 100 years. J Eukaryot Microbiol 2008;55(6):467-475. https://doi.org/10.1111/j.1550-7408.2008.00345.x
- 7. Galeh TM, Sarvi S, Hosseini SA, Daryani A. Genetic diversity of Toxoplasma gondii isolates from rodents in the world: a systematic review. Transbound Emerg Dis 2022;69(3):943-957. https://doi.org/10.1111/tbed.14096
- 8. Prandota J. Autism spectrum disorders may be due to cerebral toxoplasmosis associated with chronic neuroinflammation causing persistent hypercytokinemia that resulted in an increased lipid peroxidation, oxidative stress, and depressed metabolism of endogenous and exogenous substances. Res Autism Spectr Disord 2010;4(2):119-155. https://doi.org/10.1016/j.rasd.2009.09.011
- 9. Carruthers VB, Suzuki Y. Effects of Toxoplasma gondii infection on the brain. Schizophr Bull 2007;33(3):745-751. https://doi.org/10.1093/schbul/sbm008
- 10. Schlüter D, Barragan A. Advances and challenges in understanding cerebral toxoplasmosis. Front Immunol 2019;10:242. https://doi.org/10.3389/fimmu.2019.00242
- 11. Flegr J. Neurological and neuropsychiatric consequences of chronic Toxoplasma infection. Curr Clin Microbiol Rep 2015;2:163-172. https://doi.org/10.1007/s40588-015-0024-0
- 12. Syn G, Anderson D, Blackwell JM, Jamieson SE. Epigenetic dysregulation of host gene expression in Toxoplasma infection with specific reference to dopamine and amyloid pathways. Infect Genet Evol 2018;65:159-162. https://doi.org/10.1016/j.meegid.2018.07.034
- 13. Wang T, Sun X, Qin W, Zhang X, Wu L, et al. From inflammatory reactions to neurotransmitter changes: implications for understanding the neurobehavioral changes in mice chronically infected with Toxoplasma gondii. Behav Brain Res 2019;359:737-748. https://doi.org/10.1016/j.bbr.2018.09.011
- 14. Omar SSC, Moklas MAM, Mohtarrudin N, Osman M. Toxoplasma gondii stimulates the behavioural changes of rodents: updated evidence. J Med Biomed Appl Sci 2018;6(9):148-153.
- 15. Parlog A, Schlüter D, Dunay IR. Toxoplasma gondii-induced neuronal alterations. Parasite Immunol 2015;37(3):159-170. https://doi.org/10.1111/pim.12157
- 16. da Silva RC, Langoni H. Toxoplasma gondii: host-parasite interaction and behavior manipulation. Parasitol Res 2009;105(4):893-898. https://doi.org/10.1007/s00436-009-1526-6
- 17. Flegr J. Effects of Toxoplasma on human behavior. Schizophr Bull 2007;33(3):757-760. https://doi.org/10.1093/schbul/sbl074
- 18. Webster JP. The effect of Toxoplasma gondii on animal behavior: playing cat and mouse. Schizophr Bull 2007;33(3):752-756. https://doi.org/10.1093/schbul/sbl073
- 19. Al Malki JS, Hussien NA, Al Malki F. Maternal toxoplasmosis and the risk of childhood autism: serological and molecular small-scale studies. BMC Pediatr 2021;21(1):133. https://doi.org/10.1186/s12887-021-02604-4
- 20. Al-Hussainy NH, Al-Saedi AM, Al-Lehaibi JH, Al-Lehaibi YA, Al-Sehli YM, et al. Serological evidences link toxoplasmosis with schizophrenia and major depression disorder. J Microsc Ultrastruct 2015;3(3):148-153. https://doi.org/10.1016/j.jmau.2015.03.006
- 21. Alvarado-Esquivel C, Urbina-Álvarez JD, Estrada-Martínez S, Torres-Castorena A, Molotla-de-León G, et al. Toxoplasma gondii infection and schizophrenia: a case control study in a low Toxoplasma seroprevalence Mexican population. Parasitol Int 2011;60(2):151-155. https://doi.org/10.1016/j.parint.2010.12.003
- 22. Okusaga O, Langenberg P, Sleemi A, Vaswani D, Giegling I, et al. Toxoplasma gondii antibody titers and history of suicide attempts in patients with schizophrenia. Schizophr Res 2011;133(1–3):150-155. https://doi.org/10.1016/j.schres.2011.08.006
- 23. Miman O, Mutlu EA, Ozcan O, Atambay M, Karlidag R, et al. Is there any role of Toxoplasma gondii in the etiology of obsessive-compulsive disorder? Psychiatry Res 2010;177(1–2):263-265. https://doi.org/10.1016/j.psychres.2009.12.013
- 24. Tedla Y, Shibre T, Ali O, Tadele G, Woldeamanuel Y, et al. Serum antibodies to Toxoplasma gondii and Herpesvidae family viruses in individuals with schizophrenia and bipolar disorder: a case-control study. Ethiop Med J 2011;49(3):211-220.
- 25. Prandota J, Elleboudy NAF, Ismail KA, Zaki OK, Shehata HH. Increased seroprevalence of chronic toxoplasmosis in autistic children: special reference to the pathophysiology of IFN-γ and NO overproduction. Int J Neurol Res 2015;1(3):102-122.
- 26. Ramezani M, Shojaii M, Asadollahi M, Karimialavijeh E, Gharagozli K. Seroprevalence of Toxoplasma gondii in Iranian patients with idiopathic Parkinson’s disease. Clin Exp Neuroimmunol 2016;7(4):361-365. https://doi.org/10.1111/cen3.12329
- 27. Miman O, Kusbeci OY, Aktepe OC, Cetinkaya Z. The probable relation between Toxoplasma gondii and Parkinson’s disease. Neurosci Lett 2010;475(3):129-131. https://doi.org/10.1016/j.neulet.2010.03.057
- 28. Pfefferkorn ER. Interferon gamma blocks the growth of Toxoplasma gondii in human fibroblasts by inducing the host cells to degrade tryptophan. Proc Natl Acad Sci U S A 1984;81(3):908-912. https://doi.org/10.1073/pnas.81.3.908
- 29. Stibbs HH. Changes in brain concentrations of catecholamines and indoleamines in Toxoplasma gondii infected mice. Ann Trop Med Parasitol 1985;79(2):153-157. https://doi.org/10.1080/00034983.1985.11811902
- 30. Engin AB, Dogruman-Al F, Ercin U, Celebi B, Babur C, et al. Oxidative stress and tryptophan degradation pattern of acute Toxoplasma gondii infection in mice. Parasitol Res 2012;111(4):1725-1730. https://doi.org/10.1007/s00436-012-3015-6
- 31. Fujigaki S, Saito K, Takemura M, Maekawa N, Yamada Y, et al. L-tryptophan-L-kynurenine pathway metabolism accelerated by Toxoplasma gondii infection is abolished in gamma interferon-gene-deficient mice: cross-regulation between inducible nitric oxide synthase and indoleamine-2, 3-dioxygenase. Infect Immun 2002;70(2):779-786. https://doi.org/10.1128/iai.70.2.779-786.2002
- 32. Silva NM, Rodrigues CV, Santoro MM, Reis LF, Alvarez-Leite JI, et al. Expression of indoleamine 2, 3-dioxygenase, tryptophan degradation, and kynurenine formation during in vivo infection with Toxoplasma gondii: induction by endogenous gamma interferon and requirement of interferon regulatory factor 1. Infect Immun 2002;70(2):859-868. https://doi.org/10.1128/IAI.70.2.859-868.2002
- 33. Brooks JM, Carrillo GL, Su J, Lindsay DS, Fox MA, et al. Toxoplasma gondii infections alter GABAergic synapses and signaling in the central nervous system. mBio 2015;6(6):e01428-15. https://doi.org/10.1128/mBio.01428-15
- 34. Tonin AA, Da Silva AS, Thomé GR, Sangoi MB, Oliveira LS, et al. Influence of toxoplasmosis on acetylcholinesterase activity, nitric oxide levels and cellular lesion on the brain of mice. Pathol Res Pract 2014;210(8):526-532. https://doi.org/10.1016/j.prp.2014.04.025
- 35. AL-Hadad MTS, Kadhim RA, Al-Rubaye AF. Effect of chronic toxoplasmosis on levels of some neurotransmitters (dopamine, adrenaline, and noradrenaline) in human serum. J Pharm Sci Res 2019;11(2):402-405.
- 36. Atmaca HT. Expression of serotonin 2A, 2C, 6 and 7 receptor and IL-6 mRNA in experimental toxoplasmic encephalitis in mice. Heliyon 2019;5(11):e02890. https://doi.org/10.1016/j.heliyon.2019.e02890
- 37. Carrillo GL, Ballard VA, Glausen T, Boone Z, Teamer J, et al. Toxoplasma infection induces microglia-neuron contact and the loss of perisomatic inhibitory synapses. Glia 2020;68(10):1968-1986. https://doi.org/10.1002/glia.23816
- 38. Machado VS, Bottari NB, Baldissera MD, Rech VC, Ianiski FR, et al. Diphenyl diselenide supplementation in infected mice by Toxoplasma gondii: protective effect on behavior, neuromodulation and oxidative stress caused by disease. Exp Parasitol 2016;169:51-58. https://doi.org/10.1016/j.exppara.2016.07.006
- 39. David CN, Frias ES, Szu JI, Vieira PA, Hubbard JA, et al. GLT-1-dependent disruption of CNS glutamate homeostasis and neuronal function by the protozoan parasite Toxoplasma gondii. PLoS Pathog 2016;12(6):e1005643. https://doi.org/10.1371/journal.ppat.1005643
- 40. Halonen SK. Immune response to Toxoplasma gondii in the central nervous system. In Lindsay DS, Weiss LM eds, Opportunistic Infections: Toxoplasma, Sarcocystis, and Microsporidia. Springer; Boston, USA. 2004, pp 67-88.
- 41. Vargas DL, Nascimbene C, Krishnan C, Zimmerman AW, Pardo CA. Neuroglial activation and neuroinflammation in the brain of patients with autism. Ann Neurol 2005;57(1):67-81. https://doi.org/10.1002/ana.20315
- 42. Croonenberghs J, Wauters A, Devreese K, Verkerk R, Scharpe S, et al. Increased serum albumin, gamma globulin, immunoglobulin IgG, and IgG2 and IgG4 in autism. Psychol Med 2002;32(8):1457-1463. https://doi.org/10.1017/S0033291702006037
- 43. Spiroski M, Trajkovski V, Trajkov D, Petlichkovski A, Efinska-Mladenovska O, et al. Family analysis of immunoglobulin classes and subclasses in children with autistic disorder. Bosn J Basic Med Sci 2009;9(4):283-289. https://doi.org/10.17305/bjbms.2009.2780
- 44. Heuer L, Ashwood P, Schauer J, Goines P, Krakowiak P, et al. Reduced levels of immunoglobulin in children with autism correlates with behavioral symptoms. Autism Res 2008;1(5):275-283. https://doi.org/10.1002/aur.42
- 45. Warren RP, Odell JD, Warren WL, Burger RA, Maciulis A, et al. Brief report: immunoglobulin A deficiency in a subset of autistic subjects. J Autism Dev Disord 1997;27(2):187-192. https://doi.org/10.1023/a:1025895925178
- 46. Trajkovski V, Ajdinski L, Spiroski M. Plasma concentration of immunoglobulin classes and subclasses in children with autism in the Republic of Macedonia: retrospective study. Croat Med J 2004;45(6):746-749.
- 47. Trajkovski V, Petlichkovski A, Efinska-Mladenovska O, Trajkov D, Arsov T, et al. Higher plasma concentration of food-specific antibodies in persons with autistic disorder in comparison to their siblings. Focus Autism Other Dev Disabil 2008;23(3):176-185. https://doi.org/10.1177/1088357608320413
- 48. Nayeri T, Sarvi S, Moosazadeh M, Hosseininejad Z, Sharif M, et al. Relationship between toxoplasmosis and autism: a systematic review and meta-analysis. Microb Pathog 2020;147:104434. https://doi.org/10.1016/j.micpath.2020.104434
- 49. Rorman E, Zamir CS, Rilkis I, Ben-David H. Congenital toxoplasmosis: prenatal aspects of Toxoplasma gondii infection. Reprod Toxicol 2006;21(4):458-472. https://doi.org/10.1016/j.reprotox.2005.10.006
- 50. Robert-Gangneux F, Dardé ML. Epidemiology of and diagnostic strategies for toxoplasmosis. Clin Microbiol Rev 2012;25(2):264-296. https://doi.org/10.1128/CMR.05013-11
- 51. Fricker-Hidalgo H, Bailly S, Brenier-Pinchart MP, Dard C, Jean D, et al. How to estimate time of infection with Toxoplasma gondii in pregnant women. Use of specific IgG and IgM kinetics by 7 techniques on 691 sera. Diagn Microbiol Infect Dis 2020;96(4):114987. https://doi.org/10.1016/j.diagmicrobio.2020.114987
- 52. Bakunina N, Pariante CM, Zunszain PA. Immune mechanisms linked to depression via oxidative stress and neuroprogression. Immunology 2015;144(3):365-373. https://doi.org/10.1111/imm.12443
- 53. Ivanova DL, Krempels R, Denton SL, Fettel KD, Saltz GM, et al. NK cells negatively regulate CD8 T cells to promote immune exhaustion and chronic Toxoplasma gondii infection. Front Cell Infect Microbiol 2020;10:313. https://doi.org/10.3389/fcimb.2020.00313
- 54. Elsheikha HM, Büsselberg D, Zhu XQ. The known and missing links between Toxoplasma gondii and schizophrenia. Metab Brain Dis 2016;31(4):749-759. https://doi.org/10.1007/s11011-016-9822-1
- 55. Krause DL, Müller N. The relationship between Tourette’s syndrome and infections. Open Neurol J 2012;6:124-128. https://doi.org/10.2174/1874205X01206010124
- 56. Radoń-Pokracka M, Piasecki M, Lachowska A, Baczkowski S, Spaczyńska J, et al. Assessment of the implementation of the infectious diseases screening programmes among pregnant women in the Lesser Poland region and comparison with similar programmes conducted in other European Union countries. Ginekol Pol 2017;88(3):151-155. https://doi.org/10.5603/GP.a2017.0029
- 57. Schwartz CE. Aberrant tryptophan metabolism: the unifying biochemical basis for autism spectrum disorders? Biomark Med 2014;8(3):313-315. https://doi.org/10.2217/bmm.14.11
- 58. Spann MN, Sourander A, Surcel HM, Hinkka-Yli-Salomäki S, Brown AS. Prenatal toxoplasmosis antibody and childhood autism. Autism Res 2017;10(5):769-777. https://doi.org/10.1002/aur.1722
- 59. Kaňková S, Sulc J, Křivohlavá R, Kuběna A, Flegr J. Slower postnatal motor development in infants of mothers with latent toxoplasmosis during the first 18 months of life. Early Hum Dev 2012;88(11):879-884. https://doi.org/10.1016/j.earlhumdev.2012.07.001
- 60. Berrébi A, Assouline C, Bessières MH, Lathière M, Cassaing S, et al. Long-term outcome of children with congenital toxoplasmosis. Am J Obstet Gynecol 2010;203(6):552e1-552.e6. https://doi.org/10.1016/j.ajog.2010.06.002
- 61. Schwarcz R, Stone TW. The kynurenine pathway and the brain: challenges, controversies and promises. Neuropharmacology 2017;112(Pt B):237-247. https://doi.org/10.1016/j.neuropharm.2016.08.003
- 62. Walther DJ, Peter JU, Bashammakh S, Hörtnagl H, Voits M, et al. Synthesis of serotonin by a second tryptophan hydroxylase isoform. Science 2003;299(5603):76. https://doi.org/10.1126/science.1078197
- 63. Mahmoud ME, Fereig R, Nishikawa Y. Involvement of host defense mechanisms against Toxoplasma gondii infection in anhedonic and despair-like behaviors in mice. Infect Immun 2017;85(4):e00007-17. https://doi.org/10.1128/IAI.00007-17
- 64. Chugani DC. Serotonin in autism and pediatric epilepsies. Ment Retard Dev Disabil Res Rev 2004;10(2):112-116. https://doi.org/10.1002/mrdd.20021
- 65. Rumsey JM, Ernst M. Functional neuroimaging of autistic disorders. Ment Retard Dev Disabil Res Rev 2000;6(3):171-179. https://doi.org/10.1002/1098-2779(2000)6:3<171::AID-MRDD4>3.0.CO;2-N
- 66. Williams K, Brignell A, Randall M, Silove N, Hazell P. Selective serotonin reuptake inhibitors (SSRIs) for autism spectrum disorders (ASD). Cochrane Database Syst Rev 2013;2013(8):CD004677. https://doi.org/10.1002/14651858.CD004677.pub3.
- 67. Anderson GM. Genetics of childhood disorders: XLV. Autism, part 4: serotonin in autism. J Am Acad Child Adolesc Psychiatry 2002;41(12):1513-1516. https://doi.org/10.1097/00004583-200212000-00025
- 68. Cook EH Jr, Charak DA, Arida J, Spohn JA, Roizen NJ, et al. Depressive and obsessive-compulsive symptoms in hyperserotonemic parents of children with autistic disorder. Psychiatry Res 1994;52(1):25-33. https://doi.org/10.1016/0165-1781(94)90117-1
- 69. Peng X, Brenner LA, Mathai AJ, Cook TB, Fuchs D, et al. Moderation of the relationship between Toxoplasma gondii seropositivity and trait impulsivity in younger men by the phenylalanine-tyrosine ratio. Psychiatry Res 2018;270:992-1000. https://doi.org/10.1016/j.psychres.2018.03.045
- 70. Volkow ND, Wang GJ, Fowler JS, Logan J, Schlyer D, et al. Imaging endogenous dopamine competition with [11C]raclopride in the human brain. Synapse 1994;16(4):255-262. https://doi.org/10.1002/syn.890160402
- 71. Köves K, Kausz M, Reser D, Horváth K. What may be the anatomical basis that secretin can improve the mental functions in autism? Regul Pept 2002;109(1–3):167-172. https://doi.org/10.1016/S0167-0115(02)00200-8
- 72. Abdoli A, Dalimi A. Are there any relationships between latent Toxoplasma gondii infection, testosterone elevation, and risk of autism spectrum disorder? Front Behav Neurosci 2014;8:339. https://doi.org/10.3389/fnbeh.2014.00339
- 73. Juanah LY, Jalaludin J, Osman M, Osman ZJ. Seroprevalence of Toxoplasma gondii among schizophrenics at Hospital Kajang. Am J Infect Dis 2013;9(1):11.
- 74. Celik T, Kartalci S, Aytas O, Akarsu GA, Gozukara H, et al. Association between latent toxoplasmosis and clinical course of schizophrenia-continuous course of the disease is characteristic for Toxoplasma gondii-infected patients. Folia Parasitol(Praha); 2015. 62:2015015 https://doi.org/10.14411/fp.2015.015
- 75. Işeri E, Güney E, Ceylan MF, Yücel A, Aral A, et al. Increased serum levels of epidermal growth factor in children with autism. J Autism Dev Disord 2011;41(2):237-241. https://doi.org/10.1007/s10803-010-1046-3
- 76. Deutsch SI, Burket JA, Urbano MR, Benson AD. The α7 nicotinic acetylcholine receptor: a mediator of pathogenesis and therapeutic target in autism spectrum disorders and Down syndrome. Biochem Pharmacol 2015;97(4):363-377. https://doi.org/10.1016/j.bcp.2015.06.005
- 77. Ray MA, Graham AJ, Lee M, Perry RH, Court JA, et al. Neuronal nicotinic acetylcholine receptor subunits in autism: an immunohistochemical investigation in the thalamus. Neurobiol Dis 2005;19(3):366-377. https://doi.org/10.1016/j.nbd.2005.01.017
- 78. McTighe SM, Neal SJ, Lin Q, Hughes ZA, Smith DG. The BTBR mouse model of autism spectrum disorders has learning and attentional impairments and alterations in acetylcholine and kynurenic acid in prefrontal cortex. PLoS One 2013;8(4):e62189. https://doi.org/10.1371/journal.pone.0062189
- 79. Bhandage AK, Barragan A. Calling in the CaValry: Toxoplasma gondii hijacks GABAergic signaling and voltage-dependent calcium channel signaling for Trojan horse-mediated dissemination. Front Cell Infect Microbiol 2019;9:61. https://doi.org/10.3389/fcimb.2019.00061
- 80. Shimmura C, Suda S, Tsuchiya KJ, Hashimoto K, Ohno K, et al. Alteration of plasma glutamate and glutamine levels in children with high-functioning autism. PLoS One 2011;6(10):e25340. https://doi.org/10.1371/journal.pone.0025340
- 81. Chao HT, Chen H, Samaco RC, Xue M, Chahrour M, et al. Dysfunction in GABA signalling mediates autism-like stereotypies and Rett syndrome phenotypes. Nature 2010;468(7321):263-269. https://doi.org/10.1038/nature09582
- 82. Nakamura K, Sekine Y, Ouchi Y, Tsujii M, Yoshikawa E, et al. Brain serotonin and dopamine transporter bindings in adults with high-functioning autism. Arch Gen Psychiatry 2010;67(1):59-68. https://doi.org/10.1001/archgenpsychiatry.2009.137
- 83. Gatkowska J, Wieczorek M, Dziadek B, Dzitko K, Dlugonska H. Sex-dependent neurotransmitter level changes in brains of Toxoplasma gondii infected mice. Exp Parasitol 2013;133(1):1-7. https://doi.org/10.1016/j.exppara.2012.10.005
- 84. Roberts CW, Cruickshank SM, Alexander J. Sex-determined resistance to Toxoplasma gondii is associated with temporal differences in cytokine production. Infect Immun 1995;63(7):2549-2555. https://doi.org/10.1128/iai.63.7.2549-2555.1995
- 85. Walker W, Roberts CW, Ferguson D, Jebbari H, Alexander J. Innate immunity to Toxoplasma gondii is influenced by gender and is associated with differences in interleukin-12 and gamma interferon production. Infect Immun 1997;65(3):1119-1121. https://doi.org/10.1128/IAI.65.3.1119-1121.1997
- 86. Lindová J, Novotná M, Havlícek J, Jozífková E, Skallová A, et al. Gender differences in behavioural changes induced by latent toxoplasmosis. Int J Parasitol 2006;36(14):1485-1492. https://doi.org/10.1016/j.ijpara.2006.07.008
- 87. Lindová J, Kubena AA, Sturcová H, Krivohlavá R, Novotná M, et al. Pattern of money allocation in experimental games supports the stress hypothesis of gender differences in Toxoplasma gondii-induced behavioural changes. Folia Parasitol (Praha) 2010;57:136-142.
- 88. Alexander J, Stimson WH. Sex hormones and the course of parasitic infection. Parasitol Today 1988;4(7):189-193. https://doi.org/10.1016/0169-4758(88)90077-4
- 89. Schuurs A, Verheul H. Effects of gender and sex steroids on the immune response. J Steroid Biochem 1990;35(2):157-172. https://doi.org/10.1016/0022-4731(90)90270-3
- 90. Kittas C, Henry L. Effect of sex hormones on the response of mice to infection with Toxoplasma gondii. Br J Exp Pathol 1980;61(6):590-600.
- 91. Werling DM, Geschwind DH. Sex differences in autism spectrum disorders. Curr Opin Neurol 2013;26(2):146-153. https://doi.org/10.1097/WCO.0b013e32835ee548
- 92. Schaafsma SM, Pfaff DW. Etiologies underlying sex differences in autism spectrum disorders. Front Neuroendocrinol 2014;35(3):255-271. https://doi.org/10.1016/j.yfrne.2014.03.006
- 93. de Giambattista C, Ventura P, Trerotoli P, Margari F, Margari L. Sex differences in autism spectrum disorder: focus on high functioning children and adolescents. Front Psychiatry 2021;12:539835. https://doi.org/10.3389/fpsyt.2021.539835
- 94. Houghton R. Utilisation and Outcomes of Treatment in Autism Spectrum Disorder [doctoral disseration]. Maastricht University; Maastricht, Netherlands. 2021, https://doi.org/10.26481/dis.20210304rh
- 95. El-Baz F, Ismael NA, El-Din SMN. Risk factors for autism: an Egyptian study. Egypt J Med Hum Genet 2011;12(1):31-38. https://doi.org/10.1016/j.ejmhg.2011.02.011
- 96. Tick B, Bolton P, Happé F, Rutter M, Rijsdijk F. Heritability of autism spectrum disorders: a meta-analysis of twin studies. J Child Psychol Psychiatry 2016;57(5):585-595. https://doi.org/10.1111/jcpp.12499
- 97. Wu S, Wu F, Ding Y, Hou J, Bi J, et al. Advanced parental age and autism risk in children: a systematic review and meta-analysis. Acta Psychiatr Scand 2017;135(1):29-41. https://doi.org/10.1111/acps.12666
- 98. Galeh TM, Ghazvini H, Mohammadi M, Sarvi S, Azizi S, et al. Effects of diverse types of Toxoplasma gondii on the outcome of Alzheimer’s disease in the rat model. Microb Pathog 2023;174:105931. https://doi.org/10.1016/j.micpath.2022.105931
- 99. Galeh TM, Ghazvini H, Sarvi S, Mohammadi M, Asgarian-Omran H, et al. Controversial effects of diverse types of Toxoplasma gondii on the anxiety-like behavior and cognitive impairments in the animal model of Alzheimer’s disease. Iran J Psychiatry Behav Sci 2022;16(3):e122961. https://doi.org/10.5812/ijpbs-122961
 , Tooran Nayeri3
, Tooran Nayeri3 , Samira Dodangeh4,#
, Samira Dodangeh4,# , Zahra Hosseininejad5,#
, Zahra Hosseininejad5,# , Asal Tanzifi6,7,#
, Asal Tanzifi6,7,# , Alireza Khalilian8
, Alireza Khalilian8 , Ahmad Daryani9,10,*
, Ahmad Daryani9,10,*