Abstract
Lymphatic filariasis due to Brugia malayi infection was endemic in several areas of South Korea. The infection was controlled, or disappeared, in most areas, with the exception of the remote southwestern islands of Jeonranam-do, including the Heugsan Islands. To discover its current situation, a small-scale survey was performed on the Heugsan Islands in September 2000. A total of 378 people, 151 male and 227 female, living in 8 villages (6 on Daeheugsan-do, 1 on Daejang-do, and 1 on Yeongsan-do) were subjected to a night blood survey for microfilaremia, and physical examination for elephantiasis on the extremities. There were 6 (1.6%) microfilaria positive cases, all in females aged 57-72 years, and from only two villages of the Daeheugsan-do area. There were 4 patients with lower leg elephantiasis, but they showed no microfilaremia. The results show that a low-grade endemicity of filariasis remains on the Daeheugsan-do.
-
Key words: Brugia malayi, microfilaria, elephantiasis, Heugsan Islands, Korea
Lymphatic filariasis was one of the important endemic diseases in Korea, and was traditionally called "Soojong-dari" (leg dropsy) (
Seo, 1978). The first authentic case was reported in an autopsy of a Korean patient demonstrating a male worm fragment in a sectioned inguinal lymph node specimen (
Yun, 1927). Thereafter, many epidemiological studies were performed, and Cheju-do (Province) (
Senoo and Lincicome, 1951;
Seo et al., 1965,
1968;
Kim et al., 1973), Kyongsangbuk-do, and Jeonranam-do (
Seo et al., 1968) were noted as the Provinces showing the highest microfilaria positive rates. Three of the major endemic areas at that time were the southern parts of Cheju-do (mainly Namcheju-gun), the eastern parts of Kyongsangbuk-do (Bongwah-gun, Andong-gun, and Yongpung-gun; formerly Yongju-gun) and the southwestern coastal areas of Jeonranam-do (Haenam-gun and Chindo-gun) (
Seo, 1978).
In the early 1970s, chemotherapeutic control programs were executed in the endemic areas of Cheju-do, with satisfactory results (
Seo, 1978;
Lee et al., 1985,
1986;
Paik et al., 1988). As to the eastern part of Kyongsangbuk-do, a spontaneous decrease of the prevalence (
Kim et al., 1977,
1980), with the complete disappearance of microfilaria positive cases (
Lee et al., 1987), was reported in Yongpung-gun. In the southwestern coastal areas of Jeonranam-do, few follow-up surveys were undertaken (
Lee et al., 1992).
In contrast, remote islands, including the Heugsan-do (Islands), were newly added as endemic areas of
B. malayi infection (
Lee et al., 1986). Subsequent surveys in the same and adjacent areas showed fairly high prevalences of microfilaremia, with considerable numbers of elephantiasis patients, up until the late 1980s (
Lee et al., 1987,
1988,
1989;
Yong et al., 1988); these areas were considered as the only remaining foci of filariasis in Korea (
Kim, 1994). Thereafter, no information has been available on the status of filariasis on the Heugsan Islands. The present study was undertaken to evaluate the present status of filariasis on the Heugsan Islands.
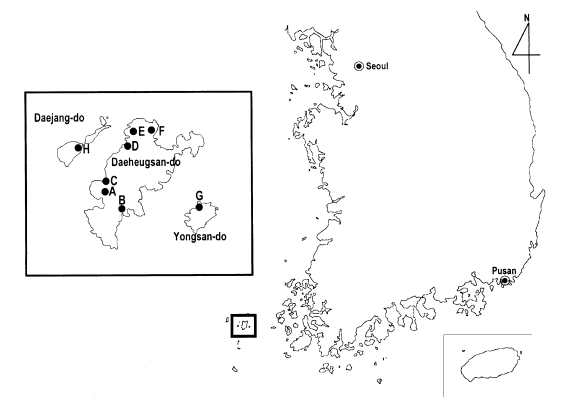
A total of 378 people, 151 male and 227 female, living in 6 villages (Shim-ri, Sa-ri, Ma-ri, Bi-ri, Gonchon-ri, and Jin-ri) of Daeheugsan-do, 1 (Jangdo-ri) of Daejang-do and 1 of Yeongsan-do (Yongsan-ri), were subjected to a night blood survey in September 2000 (
Table 1;
Fig. 1). Blood samples, 120-cmm
2, were drawn, at night (21:00-24:00), from the fingertips using a lancet and a glass pipette, coin-smeared on slides, and air-dried. These specimens were transported to our laboratory, stained with modified Giemsa (Leuko Stat solution) (Fisher Scientific, Orangeburg, New York, U.S.A.), and examined for the presence of microfilariae. At the same time, the histories on the experience of elephantiasis at extremities were taken, and brief physical examination performed on each subjected person. The microfilaria positive cases were treated with a combination therapy of 400 mg albendazole (Shinpoong Pharmaceutical Co., Seoul, Korea) and 150 µg/kg ivermectin (Shinpoong) in a single dose (
Dunyo et al., 2000a &
2000b), and followed-up 1 year later.
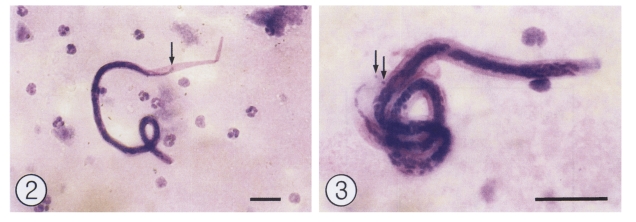
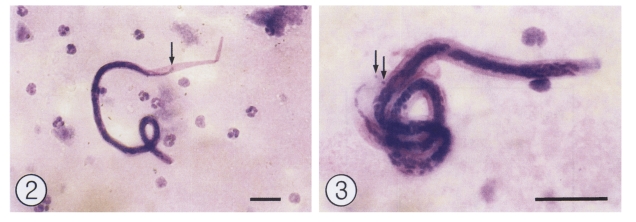
There were total 6 (1.6%) microfilaria positive cases, and were only found in two villages (Shim-ri and Sa-ri) of the Daeheugsan-do (
Table 1). All the positive cases were females, aged between the 50s and 70s (
Table 2); one was 57-years old, four were 60, 60, 62, and 63-years old, and one was 72-years old. The microfilariae were 250.8 ± 30.1 µm long and 7.5 ± 0.5 µm wide (n = 10), including the sheath, and morphologically compatible to
B. malayi, particularly with regard to the presence of terminal nuclei (
Seo, 1978) (
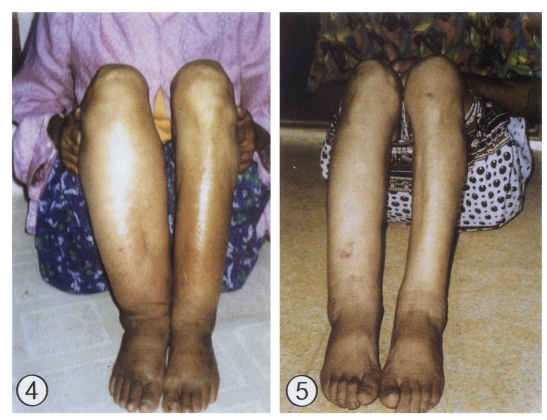
Figs. 2 & 3). Lower leg elephantiasis (
Figs. 4 & 5), either unilateral or bilateral, were found in 4 patients during this survey, 2 from Jin-ri, and 1 each from Shim-ri and Sa-ri. None revealed microfilaremia. After the treatment of the 6 microfilaremia positive cases, with albendazole and ivermectin, only one case was positive for microfilaremia 1 year posttreatment.
This study revealed that the prevalence (1.6%) of filariasis, due to
B. malayi infection, on the Heugsan Islands has markedly decreased, compared with the figures (11-22%) from 15-17 years earlier (
Lee et al., 1986,
1988). For this reason, it is suggested that the status of filariasis on the Heugsan Islands has noticeably improved. However, the presence of 6 microfilaremia cases indicates the active life cycle of
B. malayi might be preserved in these villages. Therefore, keen attention should be paid to the prevalence of microfilaremia on these Islands.
The nocturnal periodicity of the microfilariae of
B. malayi was studied in 9 Korean cases, with the peak appearance around 01:30 a.m. (
Seo, 1974). In this study, the collection of blood samples was practically impossible after 24:00, as most subjected people were asleep earlier than 23:00 p.m. For this reason, the blood survey was performed a little earlier, between 21:00 and 24:00, before the peak time of microfilaremia, so a few positive cases might have been missed.
We tried a new treatment regimen for lymphatic filariasis,
Wuchereria bancrofti infection (
Dunyo et al., 2000a &
b), a combination of albendazole (400 mg) and ivermectin (150 µg/kg) in a single dose; this also appeared to be effective against
B. malayi infections, with the exception of one case. It is regretful that the number of subjects in the present study was too small to draw any significant conclusions, and more data will be required. However, the regimen was convenient to administer, and no treated patients complained of any special adverse effects.
Notes
-
This study was supported by a grant from the Korea Association of Health Promotion (2000).
References
- 1. Dunyo SK, Nkrumah FK, Simonsen PE. A randomized double-blind placebo-controlled field trial of ivermectin and albendazole alone and in combination for the treatment of lymphatic filariasis in Ghana. Trans R Soc Trop Med Hyg 2000a;94:205-211.
- 2. Dunyo SK, Nkrumah FK, Simonsen PE. Single-dose treatment of Wuchereria bancrofti infections with ivermectin and albendazole alone or in combination: evaluation of the potential for control at 12 months after treatment. Trans R Soc Trop Med Hyg 2000b;94:437-443.
- 3. Kim DC. Lymphatic filariasis in the Republic of Korea. Yonsei Rep Trop Med 1994;25:1-12.
- 4. Kim DC, Lee OY, Lee KW. Epidemiology of malayan filariasis of inland Korea. I. Endemicity of filariasis malayi in Yongju area. Yonsei Rep Trop Med 1977;8:9-22.
- 5. Kim DC, Lee OY, Jeong EB, Jeong MG. Natural transition of endemicity of malayan filariasis in inland Korea. Rep NIH Korea 1980;17:395-404. (in Korean).
- 6. Kim JS, Lee WY, Chun SL. Ecology of filariasis on Cheju island. Korean J Parasitol 1973;11:33-53.
- 7. Lee JS, Kim TS, Lee WJ, et al. Epidemiological studies of filariasis malayi on the southern islands in Korea (III). Rep NIH Korea 1992;29:114-122. (in Korean).
- 8. Lee OY, Lee JS, Kim TS, et al. Epidemiological studies on filariasis malayi on Cheju Do. Rep NIH Korea 1985;22:241-253. (in Korean).
- 9. Lee OY, Lee JS, Kim TS, et al. Epidemiological studies on filariasis malayi on Cheju Do and the southern islands. Rep NIH Korea 1986;23:407-422. (in Korean).
- 10. Lee OY, Lee JS, Kim TS, et al. Epidemiological studies on filariasis malayi on the southern islands and inland Korea. Rep NIH Korea 1987;24:519-538. (in Korean).
- 11. Lee OY, Lee JS, Yong TS, et al. Epidemiological studies of filariasis malayi on the southern islands Korea. Rep NIH Korea 1988;25:411-425. (in Korean).
- 12. Lee OY, Lee JS, Kim TS, et al. Epidemiological studies of filariasis malayi on the southern islands of Korea (II). Rep NIH Korea 1989;26:247-265. (in Korean).
- 13. Paik YH, Cho YJ, Koo DS, Ree HI, Shim JC. Studies on the current epidemiological situation of brugian filariasis in endemic areas of Korea. Korean J Parasitol 1988;26:255-262.
- 14. Senoo T, Lincicome DR. Malayan filariasis, incidence and distribution in southern Korea. US Armed Forces Med J 1951;2:1483-1489.
- 15. Seo BS, Rim HJ, Seong SH, Park YH, Kim BC, Lim TB. The epidemiological studies on the filariasis in Korea. I. Filariasis in Cheju-Do (Quelpart-island). Korean J Parasitol 1965;3:139-145. (in Korean).
- 16. Seo BS, Rim HJ, Lim YC, Kang IK, Park YO. The epidemiological studies on the filariasis in Korea. II. Distribution and prevalence of malayan filariasis in southern Korea. Korean J Parasitol 1968;6:132-141.
- 17. Seo BS. The periodicity of microfilariae of Brugia malayi in Cheju Island, Korea. Korean J Parasitol 1974;12:95-100.
- 18. Seo BS. Malayan filariasis in Korea. Korean J Parasitol 1978;16(suppl):1-108.
- 19. Yong TS, Lee OY, Lee JS, Kim TS, Kim DC. Clinical observation of malayan filariasis cases on the Heugsan Islands, Korea. Rep NIH Korea 1988;25:427-441. (in Korean).
- 20. Yun IS. Elephantiasis due to filaria in Korea. Chosen Iggakai Zasshi 1927;76:326-334. (in Japanese).
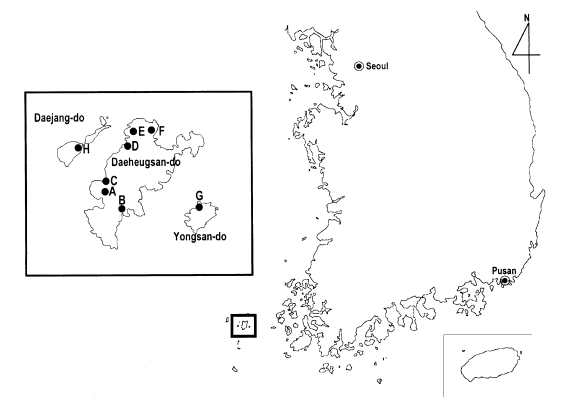
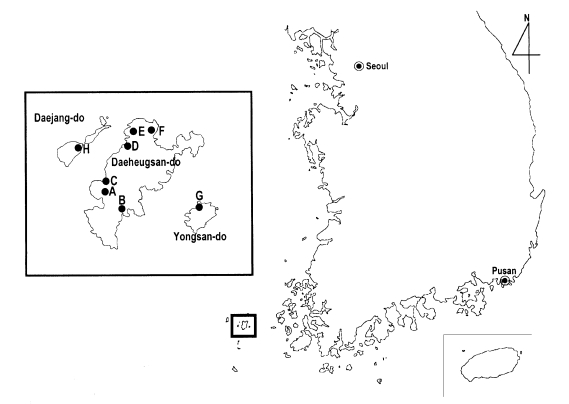
Fig. 1Map of the Heugsan Islands (boxes) showing the areas surveyed for Brugia malayi infections. A: Shim-ri, B: Sa-ri, C: Gonchon-ri, D: Bi-ri, E: Ma-ri, F: Jin-ri, G: Yongsna-ri, and H: Jangdo-ri. Positive microfilaremia cases were found in the villages A (4 cases) and B (2 cases).
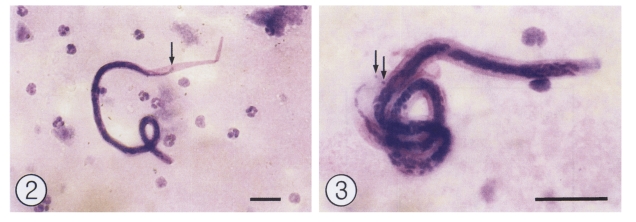
Figs. 2-3Microfilariae of Brugia malayi in the blood of patients on Daeheugsan-do. Modified Giemsa stain. Bar = 20 µm. Fig. 2. High dry lens view (× 400) of a microfilaria. The arrow indicates a terminal nucleus. Fig. 3. Oil immersion lens view (× 1,000) of another microfilaria. Arrows indicate terminal nuclei.
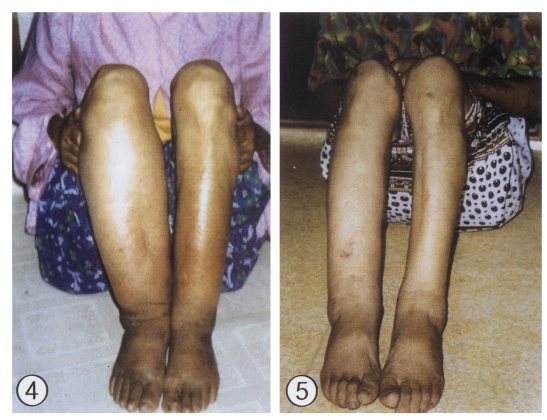
Figs. 4-5Elephantiasis of lower legs in the patients residing on Daeheugsan-do. Fig. 4. Bilateral elephantiasis of lower legs in a 70-year-old woman. She had a history of swollen legs for over 25 years. Fig. 5. Bilateral elephantiasis of the lower legs in a 67-year-old woman, who has suffered from the disease for 20 years.
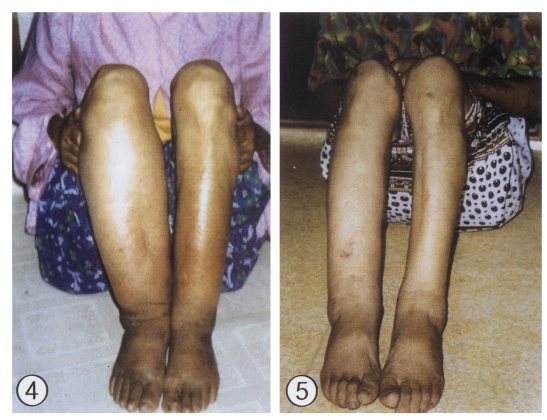
Table 1.Microfilaria positive cases among people on the Heugsan Islands (September 2000)
Table 1.
|
Village codea)
|
Village name |
No. people examined
|
No. positive for microfilaria (%)
|
|
Males |
Females |
Total |
Males |
Females |
Total |
|
A |
Shim-ri |
16 |
28b)
|
44 |
0 (0.0) |
4 (14.2) |
4 (8.8) |
|
B |
Sa-ri |
30 |
46b)
|
76 |
0 (0.0) |
2 (4.3) |
2 (2.6) |
|
C |
Gonchon-ri |
14 |
10 |
24 |
0 (0.0) |
0 (0.0) |
0 (0.0) |
|
D |
Bi-ri |
19 |
27 |
46 |
0 (0.0) |
0 (0.0) |
0 (0.0) |
|
E |
Ma-ri |
9 |
18 |
27 |
0 (0.0) |
0 (0.0) |
0 (0.0) |
|
F |
Jin-ri |
30 |
43b)
|
73 |
0 (0.0) |
0 (0.0) |
0 (0.0) |
|
G |
Yongsan-ri |
16 |
29 |
45 |
0 (0.0) |
0 (0.0) |
0 (0.0) |
|
H |
Jangdo-ri |
16 |
29 |
45 |
0 (0.0) |
0 (0.0) |
0 (0.0) |
|
Total |
151 |
229 |
380 |
0 (0.0) |
6 (2.6) |
6 (1.6) |
Table 2.Prevalence of microfilaremia among people on the Heugsan Islands by age and sex
Table 2.
|
Age group |
Males
|
Females
|
Total
|
|
No. exam. |
No. posit. (%) |
No. exam. |
No. posit. (%) |
No. exam. |
No. posit. (%) |
|
0-9 |
6 |
0 (0.0) |
9 |
0 (0.0) |
15 |
0 (0.0) |
|
10-19 |
8 |
0 (0.0) |
15 |
0 (0.0) |
23 |
0 (0.0) |
|
20-29 |
16 |
0 (0.0) |
7 |
0 (0.0) |
23 |
0 (0.0) |
|
30-39 |
19 |
0 (0.0) |
15 |
0 (0.0) |
34 |
0 (0.0) |
|
40-49 |
20 |
0 (0.0) |
27 |
0 (0.0) |
47 |
0 (0.0) |
|
50-59 |
23 |
0 (0.0) |
44 |
1 (2.3) |
67 |
1 (1.5) |
|
60-69 |
40 |
0 (0.0) |
60 |
4 (6.7) |
100 |
4 (4.0) |
|
70 & over |
20 |
0 (0.0) |
48 |
1 (2.1) |
68 |
1 (1.5) |
|
Unknown |
1 |
0 (0.0) |
2 |
0 (0.0) |
3 |
0 (0.0) |
|
Total |
153 |
0 (0.0) |
227 |
6 (2.6) |
380 |
6 (1.6) |
Citations
Citations to this article as recorded by

- Prevention and Control Strategies for Parasitic Infections in the Korea Centers for Disease Control and Prevention
Young Yil Bahk, Eun-Hee Shin, Shin-Hyeong Cho, Jung-Won Ju, Jong-Yil Chai, Tong-Soo Kim
The Korean Journal of Parasitology.2018; 56(5): 401. CrossRef - Follow-up Study of Patients Previously Diagnosed with Lymphatic Filariasis in Korea
Hyeng Il Cheun, Hee Eun Shin, Da Won Ma, Sung Hee Hong, Tae Yun Kim, Sang Eun Lee, JungWon Ju, Yun-Kyu Park, Tong-Soo Kim, Shin Hyeong Cho
Osong Public Health and Research Perspectives.2017; 8(6): 421. CrossRef - Surveillance and Vector Control of Lymphatic Filariasis in the Republic of Korea
Shin Hyeong Cho, Da Won Ma, Bo Ra Koo, Hee Eun Shin, Wook Kyo Lee, Byong Suk Jeong, Chaeshin Chu, Won Ja Lee, Hyeng Il Cheun
Osong Public Health and Research Perspectives.2012; 3(3): 145. CrossRef - Seasonal Prevalence of Mosquitoes, Including Vectors of Brugian Filariasis, in Southern Islands of the Republic of Korea
Hyeng-Il Cheun, Shin-Hyeong Cho, Hee-Il Lee, E-Hyun Shin, Jong-Soo Lee, Tong-Soo Kim, Won-Ja Lee
The Korean Journal of Parasitology.2011; 49(1): 59. CrossRef - Elimination of lymphatic filariasis in the Republic of Korea: an epidemiological survey of formerly endemic areas, 2002–2006
Hyeong‐Il Cheun, Jong‐Soo Lee, Shin‐Hyeong Cho, Yoon Kong, Tong‐Soo Kim
Tropical Medicine & International Health.2009; 14(4): 445. CrossRef - Review of Zoonotic Parasites in Medical and Veterinary Fields in the Republic of Korea
Heejeong Youn
The Korean Journal of Parasitology.2009; 47(Suppl): S133. CrossRef - Successful Control of Lymphatic Filariasis in the Republic of Korea
Hyeng-Il Cheun, Yoon Kong, Shin-Hyeong Cho, Jong-Soo Lee, Jong-Yil Chai, Joo-Shil Lee, Jong-Koo Lee, Tong-Soo Kim
The Korean Journal of Parasitology.2009; 47(4): 323. CrossRef - Trends in parasitic diseases in the Republic of Korea
Eun-Hee Shin, Sang-Mee Guk, Hyo-Jin Kim, Soon-Hyung Lee, Jong-Yil Chai
Trends in Parasitology.2008; 24(3): 143. CrossRef